Last updated: July 27, 2020
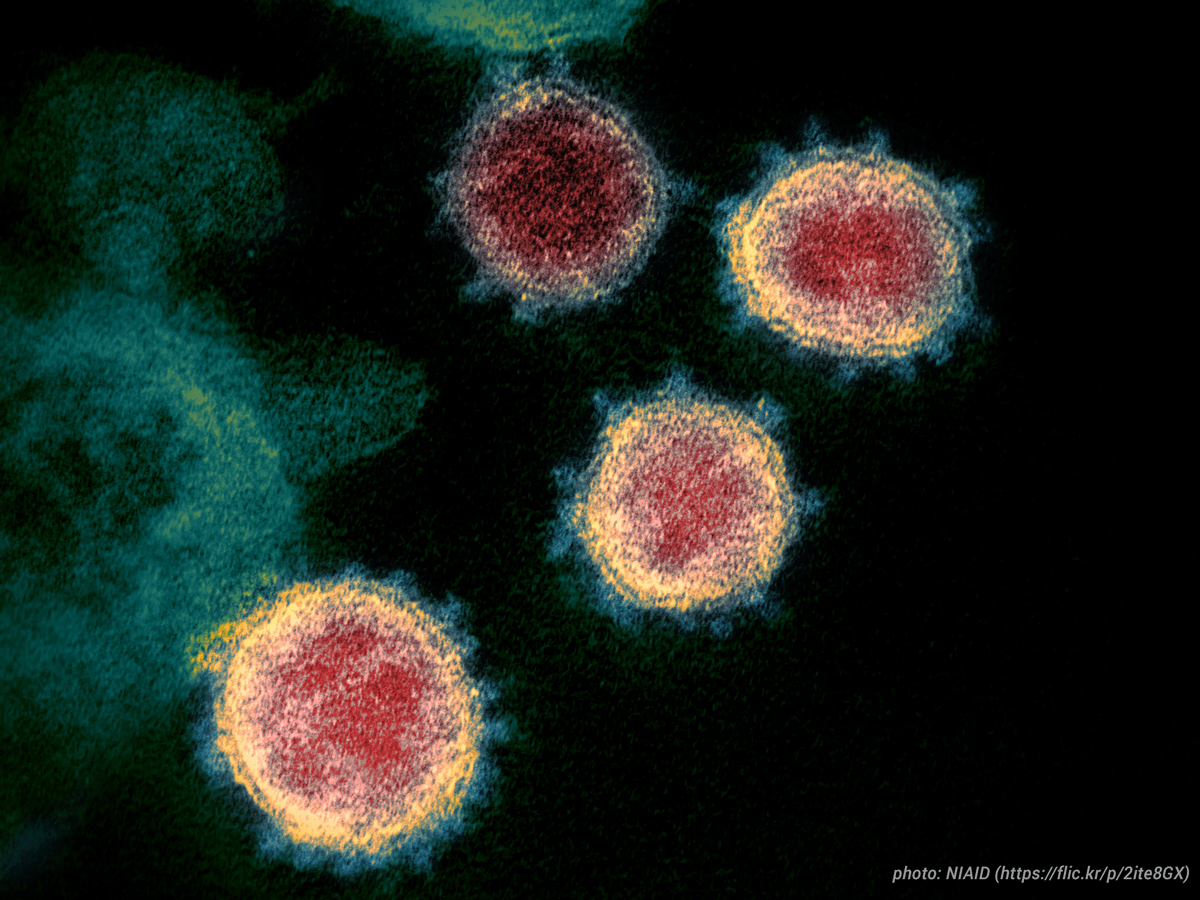
The Novel Coronavirus (SARS-CoV-2) has resulted in over 15.7 million cases of the COVID-19 disease, with more than 640,000 deaths to date. The World Health Organization declared on March 11 that it is a global pandemic. See the latest World Health Organization situation reports. Visit ICAP’s COVID-19 news and resources page for the latest information and updates.
February 1: Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, is quoted in a recent Politico article expressing her concerns about data being overlooked when officials consider new steps and restrictions to stop the spread of COVID-19.
“I feel like people are numbed by the numbers; I worry about the complacency and fatigue,” said El-Sadr. “I worry about the focus on vaccines, rather than what’s happening with the virus.”
February 1: Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, is quoted an article in the New York Times expressing her concern on the continued spread of the virus.
February 1: ICAP’s Wafaa El-Sadr, MD, MPH, MPA, stresses the importance of widespread surveillance to stop the spread of COVID-19 due to inequitable distribution and inconsistent price points over the course of the epidemic on ABC News.
“You’ll miss some, but you’ll catch others and you’ll catch them early so you can isolate them rapidly and do the contact tracing very promptly as well,” said El-Sadr of COVID-19 rapid tests. “There are situations where in parts of this country there’s not the luxury of having PCR testing.”
January 27: A look back at how ICAP mobilized to meet the COVID-19 pandemic in its 30-plus countries of operation.
January 22: In this expansive conversation on the podcast Inspired Service, Yen Pottinger–senior lab advisor at ICAP and former HIV Incidence Team lead at the CDC–explores the science of the virus itself, the role of the public sector as a first mover in the health sector, and how to best harness the goodwill of the American people.

January 19: In a bold Opinion piece published in the New York Times and co-authored by ICAP’s global director, Wafaa El-Sadr
January 8: As COVID-19 claims more lives, ICAP’s Jessica Justman advocates for the rapid roll out of a vaccine to the public in an article in The Guardian.
“Hundreds of thousands of people are dying and the roll out of the vaccine needs to happen as quickly as possible.”
January 7: ICAP’s Yen Pottinger featured in a feature story in The New Yorker examining America’s missteps in battling the coronavirus.
December 21: ICAP’s Wafaa El-Sadr, MD, MPH, MPA, explains the science behind the Moderna and Pfizer COVID-19 vaccines and answers commonly asked questions on Al-Jazeera.
“They’re similar in that they both use the same technology, the same approach to making the vaccine. They both require two doses. These two vaccines work incredibly well.”
July 27: Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, is quoted in an article in Insider Magazine on school reopening and how to mitigate COVID-19 risk:
Wafaa El-Sadr, a professor of epidemiology and medicine and the director of ICAP at Columbia University’s Mailman School of Public Health, said schools should be screening for illnesses among students and staff, lower classroom densities, space out desks, and require face masks if they want to accurately adhere to public health measures.
But before that, she told Insider, they must evaluate the status of COVID-19 in their community and determine whether or not it would be a risk to reopen schools.
“The risk is dependent on transmission risk in the community and transmission risk in the school,” El-Sadr said. “Schools have to take into account the situation in their communities as they decide what to do.”
July 25: Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP at Columbia University, is quoted in a New York Times article on how to assess and mitigate COVID-19 risk while receiving hair and beauty treatments:
Should you decide to venture out, you may be wondering how to stay safer during a haircut, wax or manicure. “It’s reducing the risk, not eliminating the risk,” said Wafaa El-Sadr, a professor of epidemiology and medicine at Columbia University’s Mailman School of Public Health. “Nobody can tell you it’s safe to do x, y and z. We can make x, y and z as safe as possible.”
July 24: Jessica Justman, MD, ICAP’s senior technical director, spoke on NPR’s All Things Considered, discussing current efforts to determine whether blood serum taken from recovered COVID-19 patients could help prevent the disease in others.
July 22: Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP at Columbia University, is quoted in a New York Times article on the new guidelines from the U.S. Centers for Disease Control and Prevention (CDC) saying that recovering coronavirus patients should be free to resume normal activity after 10 days, if they have no fever or other symptoms:
“This is anchored in evidence,” said Dr. Wafaa El-Sadr, professor of epidemiology at the Mailman School of Public Health at Columbia University. “I think it makes sense.”
Also on July 22, ICAP co-hosted a special webinar titled “Phylogeny and COVID-19: Shedding light on origin and transmission of SARS-CoV-2” with Treatment Action Group and COVID-19 Working Group-New York. The session was moderated by Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP, and featured Bette Korber, PhD, Laboratory Fellow and Scientist in Theoretical Biology and Biophysics at the Los Alamos National Laboratory, and Joel Wertheim, PhD, Associate Professor of Medicine at the University of California San Diego.
July 20: Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP at Columbia University, spoke to Al Jazeera about the experimental coronavirus vaccine developed by scientists at Oxford University, which has been shown in an early trial to prompt a protective immune response in hundreds of people who got the shot:
“This is very exciting news, encouraging news, that we now have another vaccine that is poised to move into phase three studies, which are the definitive studies that will tell us if the vaccine works, and if it is safe in large numbers of participants. […] We have to be very cautious because while this phase one-two study was done in a little more than a thousand participants, sometimes you need to study a vaccine in a much larger population in order to see rare side effects. I think it’s important for us to move ahead to larger studies that will recruit maybe 30,000 individuals, and hope that some rare side effect does not manifest itself once you’re using it in a larger population.”
July 15: Jessica Justman, MD, ICAP’s senior technical director, spoke to WNYC, discussing the need for social distancing even while outdoors, in order to curb the spread of COVID-19.
“Try to pay attention to the six foot guidance, which might be hard to do,” she said. “But even outdoors, you still want to keep a distance for people.”
Also on July 15, Dr. Justman is quoted in an Insider Magazine article on the safety of ‘backyard summer camps’ popping up as an alternative to regular summer camps that may be closed or at reduced capacity due to COVID-19:
The safety of each camp will ultimately “depend on who attends,” Jessica Justman, an epidemiologist and associate professor of medicine at Columbia University’s Mailman School of Public Health, told Insider in an email.
“If the children are all from one family or are already clustering together in one ‘bubble,’ then the main safety issue to consider will be the organizers/counselors’ health as they will be exposed to the children,” Justman said. “If the children come from different families and do not normally spend time together, then the safety concerns will expand in proportion to the size of the new ‘pod.’”
Since each camper will go back home at the end of the day, they risk giving the virus to members of their families, Justman said.
July 13: Jessica Justman, MD, ICAP’s senior technical director, is quoted in a CNN Health article on effective public health messaging to reduce the spread of COVID-19:
Dr. Jessica Justman, an infectious diseases specialist and epidemiologist at Columbia University and attending physician at the Columbia University Irving Medical Center, says that messaging plays an important role in the implementation of public health strategies, like this one. She says that it can make a difference when a leader dons a face mask as an example to others.
Justman says it can also be helpful to have celebrities help disseminate important public health messages, because they are often regarded as opinion leaders in our society.
July 10: Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP at Columbia University, is quoted in a CNN Health article on the potential use of BCG, a common vaccine used globally for tuberculosis prevention, to fight COVID-19:
“The nice thing is that it’s given only once. It’s potentially quite feasible to scale up production of the vaccine, if it works and it’s safe,” said Dr. Wafaa El-Sadr, a Columbia University professor of epidemiology and director of ICAP, a global health program.
July 5: Jessica Justman, MD, ICAP’s senior technical director, is quoted in an NBC News article on summer camps and the risk for COVID-19:
“I think that with the increasing number of cases in so many states now, I am more concerned than I was before about the feasibility of summer camp,” Dr. Jessica Justman, an epidemiologist and associate professor of medicine at Columbia University’s Irving Medical Center, said in an interview.
“These things do always come down to individual judgments and decisions that parents have to make,” she said.
July 1: Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP at Columbia University, is quoted in a New York Times article on whether mass protests in response to the police killing of George Floyd might have sparked a second wave of COVID-19:
The lockdown enacted in March worked. By the end of May, when the protests began, the virus was not as prevalent in New York as it had been when the lockdown began.
“It seems we in New York City did achieve a substantial decrease in the number of cases so that made the odds of encountering a case of Covid-19 in these protests quite low,” said Wafaa El-Sadr, an epidemiology professor at Columbia University.
June 29: Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP at Columbia University, appeared on Bloomberg Europe to discuss prevention and mitigation measures to contain COVID-19:
“This is a new epidemic, and we are learning how to tackle it, both in terms of how to control it as well as how to start up after putting in place very strong mitigation measures. I don’t think anyone has gone through anything like this before, and I think what’s really important is that we take very careful steps forward using the data that we have at our fingertips, and that we’re also cognizant that we may need to take a step backwards as well, based on what happens to the epidemic.”
June 25: Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, is quoted in an article in Fast Company stating that the ‘first wave’ of COVID-19 in the U.S. is not over, and is actually getting worse:
Experts largely agree on the goals for virus suppression. “Until we have a safe and effective vaccine that everyone takes, what needs to happen is we try and sustain this low level of transmission, which I think is a balancing act,” says Wafaa El-Sadr, an infectious disease specialist at Columbia University. She says that will involve wearing masks and limiting social contacts consistently. But she worries that, thanks to disinformation like Pence’s op-ed, public health messaging has become politicized.
“There’s this pitting of public health and economic health, but we don’t want to pit those against each other,” she says. It’s vital that people are able to get back to work, she says, but they need to wear face coverings and keep an appropriate distance from colleagues. “We need these public health measures, we need to sustain them as much as possible until we have a vaccine,” she says.
June 23: Jessica Justman, MD, ICAP’s senior technical director, is quoted in a Reuters article on a potential second wave of COVID-19 infections.
While there’s no formal definition for a second wave, some experts say they know it when they see it.
“It’s often quite clear; you’ll see a rise involving a second group of people after infections in a first group have diminished,” epidemiologist Jessica Justman of Columbia University’s Mailman School of Public Health said.
Also on June 23, Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, is quoted in an article on the Quanta Magazine website about why COVID-19 infections are relatively low in South Asia.
One hypothesis involves the BCG vaccine, which is used universally in South Asia. However, according to the article, “the WHO examined three studies still undergoing peer review in which the authors observed that countries routinely using the BCG vaccine had less incidence of COVID-19. The WHO concluded that ‘such ecological studies are prone to significant bias from many confounders,’ including differences in national demographics, testing rates for COVID-19 infections, and the stage of the pandemic in each country.”
Wafaa El-Sadr, a professor of epidemiology and medicine and the director of ICAP at Columbia University, agreed. “This is only a hypothesis, yet to be proven,” she said.
June 21: Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, spoke to NPR’s Weekend Edition Sunday about the increase in COVID-19 infections among younger people, and the need to mobilize this population to help curb the pandemic.
Dr. Wafaa El-Sadr, a professor at Columbia University’s Mailman School of Public Health, said it’s not yet clear to what extent young people are driving community transmission of the virus, but it’s a key metric that public health agencies should be following.
“It’s a lost opportunity,” she said. “I think young people can potentially have a very, very valuable role if we can harness their energy and attention.”
El-Sadr said the best strategy is to enlist “trusted spokespeople” who can help mobilize a younger population through things such as social media rather than relying on the same messaging that’s been coming from public health officials for months.
“How do we find those individuals that young people today want to emulate? The trendsetters that they will listen to and follow,” she said.
June 17: ICAP, Treatment Action Group, and COVID-19 Working Group-New York co-hosted a webinar on “Modeling of COVID-19 and Other Infectious Diseases,” moderated by Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, and featuring Jeffrey Shaman, PhD, Professor of Environmental Health Sciences at Columbia University Mailman School of Public Health, and Lauren Ancel Meyers, PhD, Cooley Centennial Professor of Integrative Biology and Statistics & Data Sciences at The University of Texas at Austin.
June 11: Jessica Justman, MD, ICAP’s senior technical director, participated in a Guardian Q&A on a potential second wave of COVID-19 infections in the U.S.
Are there still concerns that a second wave will happen in the fall?
Justman: I think a modest second wave is coming, and then contact tracing and other measures will be put in place to get on top of it. The real question is what’s going to happen in the fall. That’s why there’s a huge push to get vaccine trials running.
June 10:
Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, participated in a panel discussion, “Remembering the AIDS Crisis in the Time of COVID-19: How Lessons from One Epidemic can Guide the Response to Another,” hosted by Hunter College’s LGBTQ Policy Center at the Roosevelt House Public Policy Institute.
A write-up of the event appeared in Upper East Side local outlet Our Town:
“The emergence of the COVID pandemic resulted in rapidly trying to identify treatments and find vaccines. And this contrasts, unfortunately, with the early years of the HIV epidemic,” El-Sadr said. “Whereas we are all aware, it took a lot of battles, a lot of fighting, a lot of advocacy, particularly by gay men and their supporters, to try to move the research agenda forward.”
June 9: An article in The Guardian quotes Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, on the potential risks of U.S. states opening up while the COVID-19 pandemic is still active.
“The worrisome thing for me is that there’s a lot of fatigue in the population overall,” said Wafaa El-Sadr, professor of epidemiology at Columbia University.
“People feel they have done distancing and they are thirsting to get outside and connect with each other. If this surge requires us taking a step back, how do we convince people to do that? I feel we’ve made five steps forward and now maybe one step back.”
Also on June 9, Jessica Justman, MD, ICAP’s senior technical director, is quoted in a Newsday article on the potential for asymptomatic spread of COVID-19.
Dr. Jessica Justman, an associate professor of medicine in epidemiology at Columbia University’s Mailman School of Public Health, said although it’s clear that asymptomatic people spread the virus, “the jury is still out” on how important a factor they are.
“Are they accounting for 5% of new infections or 50% of new infections?” she asked. “It’s not so clear.”
Studies have come to different conclusions because of variations in methodology, and more research is needed on the topic, she said.
Even so, Justman said, “It behooves us to assume it’s an important factor” and for people to continue to wear masks and practice social distancing.
June 8: A Vox article quotes Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, on the impact of COVID-19 in India:
“In Asia, India is the country of most concern, due to the large population [and] vastness of the country as well as the easing of restrictions that is ongoing,” Wafaa El-Sadr, who works on epidemiology and global health at Columbia University, told me. “It is also likely that deaths are underreported particularly from rural areas.”
June 7: A Wall Street Journal article quotes Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, on the rise of COVID-19 cases in some U.S. states:
“If you take out the impact of New York, New Jersey, Connecticut and so on, you’d have a much more worrisome picture of what’s happening in the U.S.,” said Wafaa El-Sadr, an infectious-disease specialist and epidemiologist at Columbia University. “It’s a very mixed picture. In some places, we have made amazing progress, and there are other places where I remain very concerned about what’s going on.”
June 5: Jessica Justman, MD, ICAP’s senior technical director, is quoted in a Wall Street Journal article on the potential COVID-19 risks of the large protests currently happening across the U.S. in response to the killing of George Floyd.
“We could start to see some second wave activity starting as soon as next week,” said Jessica Justman, associate professor of medicine in epidemiology at the Columbia Mailman School of Public Health, noting that the pandemic has also hit black and Hispanic communities the hardest. “Will any second wave that happens have a similar racial and ethnic disparity? That really remains to be seen.”
June 3: ICAP and Columbia Global Centers | Tunis co-hosted a webinar on COVID-19 in the Eastern Mediterranean and North Africa Region, featuring panelists Rana Hajjeh, Director of Program Management, WHO/EMRO, Hechmi Louzir, Director General, Institut Pasteur in Tunis, Tunisia, and Gerardo Noto, Resident Representative, UNDP Libya.
June 2: A New York Times article on national responses to the COVID-19 pandemic quotes Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University:
Often, leaders who responded more slowly have cited the need to prioritize economic growth. But the trade-offs between the economy and public health may not actually exist, scientists and economists say: The fastest route to economic normalcy involves controlling the spread of the virus.
“There’s this false tension that exists between public health and economic health,” said Wafaa El-Sadr, an epidemiologist at Columbia University.
Also, on June 2, Columbia’s Institute for Social and Economic Research and Policy (ISERP) announced the launch of the Center for Pandemic Research (CPR) to mobilize resources and expertise vital to the study of COVID-19. Dr. El-Sadr is among the participating experts.
May 30: Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, spoke on a webinar hosted by Columbia Global Centers | Beijing.
“In the United States, we have increased our investment in high-technology care, while at the same time decreasing our investment and appreciation of public health,” she warned, “and COVID-19 has really taught us how important they both are.”
May 29: In an ABC News report on projected mortality rates in the coming months, Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University and professor of epidemiology at Columbia University, said that “it is without a doubt that unfortunately more Americans will die through the Summer” from COVID-19.
“It is inevitable that we will continue to see new infections with deaths amongst the most vulnerable populations, the elderly, the poor, African Americans, Latinx, those with other serious conditions,” she added.
May 28: WBEZ, a local Chicago NPR affiliate, quoted Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, in a story about incomplete COVID-19 data in the state of Illinois. WBEZ reported that the jobs of those who’ve contracted COVID-19 is unknown in almost 80% of cases, which could help prevent potential future outbreaks.
Dr. El-Sadr said data “should drive everything we do. Knowing where new infections are happening… This knowledge is what’s needed in order to know what to do next.”
May 27: Wafaa El-Sadr, MD, MPH, MPA, director of ICAP at Columbia University, is quoted in an AP article on the COVID-19 death toll in the U.S. exceeding 100,000 people.
Dr. Wafaa El-Sadr, director of ICAP, a global health center at Columbia University, called the U.S. death rate shocking.
“It reflects the fact that we have neglected basic fundamentals for health,” El-Sadr said. “So, now we are in this shameful situation. It is the most vulnerable people in our midst — the elderly, the poor, members of racial/ethnic minority groups — who are the ones disproportionately getting sick and dying.”
Also on May 27, Jessica Justman, MD, ICAP’s senior technical director, explained on BRIC TV’s “BHeard” program how COVID-19 has exacerbated NYC’s existing inequities to where race and income have become the greatest factors in the pandemic’s expected mortality rate.
May 22: Jessica Justman, MD, ICAP’s senior technical director, is quoted in a May 22 New York Times article on the potential COVID-19 risks of summer camps.
Day camps pose an extra unknown in terms of risk because campers and staff return to their families each night where they could be exposed or spread the virus, said Dr. Jessica Justman, an epidemiologist and professor of medicine at Columbia University’s Irving Medical Center.
“Will the amount of virus circulating in the community be low enough so that level of mixing will be OK, or will that trigger a second wave?” she said.
Also on May 22, WBUR’s “Here & Now” interviewed Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, about the state of the COVID-19 pandemic, after the number of COVID-19 cases worldwide surpassed 5 million, with most of the new cases coming from just four countries: the United States, Russia, Brazil and India.
Additionally, ICAP’s Yen Pottinger, PhD, Senior Lab Advisor for the PHIA Project, presented on SARS-CoV-2 testing for COVID Connect webinar hosted by Michigan-based company in2being.
May 21: María Lahuerta, PhD, MPH, ICAP’s deputy director of strategic information, is featured in a May 21 video interview with Valencian news outlet À Punt NTC.
Hui entrevistem María Lahuerta, experta en epidemiologia de malalties infeccioses i salut internacional en el @ICAP_ColumbiaU. ➡️Ens explicarà les claus per a combatre la #COVIDー19.
En #ÀPuntNTC migdia amb @VMaso.
⏰A les 13:55 h
🔴En directe 👉https://t.co/oSH8WZgI37 pic.twitter.com/xToAw9MQHy— À Punt NTC (@apuntnoticies) May 21, 2020
Additionally, Jessica Justman, MD, ICAP’s senior technical director, is quoted in a May 21 Bloomberg article sharing recommendations for safer travel in light of COVID-19 concerns:
Prepare to pack more than just clothes if you want to reduce your risk, as well as that of local residents. Columbia professor Justman recommends bringing your own groceries, for instance, “so you don’t have to go into a new grocery store.”
May 20: In a May 20 AP article, Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, said having doctors relay contradictory information on behalf of the president is “quite alarming.”
“I find it totally irresponsible to have physicians who are touting some information that’s not anchored in evidence and not anchored in science,” El-Sadr said. “What often creates confusion is the many voices that are out there, and many of those voices do have a political interest, which is the hugely dangerous situation we are at now.”
This article was picked up in numerous outlets, including the New York Times, and quoted in a May 20 Vanity Fair article
May 19: María Lahuerta, PhD, MPH, ICAP’s deputy director of strategic information, spoke to Spanish outlet Antena 3 about contact tracing to control the spread of COVID-19.
The epidemiologist, asked about the massive tests to control the coronavirus, is blunt: “The tests are important, but almost more important is, when we have a person diagnosed, locate their contacts so that they can be tested and isolate them . I think it is something that we do not have the capacity to do right now and that we have to reinforce, because it will be key to avoiding new outbreaks.”
Dr. Lahuerta also spoke with Spanish outlet EITB.eus about the coronavirus vaccine being developed by the Moderna company in partnership with the US National Institutes of Health.
“There will not be six million vaccines, there will have to be priority and there will be ethical debate.”
May 18: María Lahuerta, PhD, MPH, ICAP’s deputy director of strategic information, joined a panel of experts on Voice of America to discuss how close we are to a COVID-19 vaccine and whether it is time to return to normal.
Dr. Lahuerta also spoke to Spanish outlet Antena 3 about Spain’s response so far to the COVID-19 pandemic and the need for trained virus trackers to help stop the spread.
Additionally, on the May 18, 2020 broadcast of nightly news on NHK World-Japan, Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, described the emotional toll that nurses working during the COVID-19 pandemic face.
“It really is analogous to someone coming home from war. [Nurses] are witness to death and pain on a level that most people never have to witness.”
May 16: María Lahuerta, PhD, MPH, ICAP’s deputy director of strategic information, spoke to Spanish news outlet El Mundo in a May 16 interview about the global response to the COVID-19 pandemic.
We hear a lot about “test, test, test,” and without a doubt that is important, but for me it is also essential to have “data, data, data”. If you don’t know where, when, and how new infections are developing, you go into the response blind.”
May 13: ICAP co-hosted a special webinar with Treatment Action Group and the COVID-19 Working Group – New York titled “SARS-CoV-2 serological testing: What is it and what does it mean?”
ACCESS THE RECORDING (YouTube)
Also on May 13, The Zimbabwe Daily quoted Dereck Mpofu and Albert Nyathi, creators of the ICAP-commissioned COVID-19 anthem, “Apart/Together – We Stand Strong Against COVID-19,” in an article on the origins and impact of the song.
The seven-minute song blends English, Shona and Ndebele lyrics, and was made possible by a generous philanthropic gift from business leader Dr. Bing Zhao.
“Apart/Together,” with its video accompaniment, can be heard here.
May 12: Jessica Justman, MD, ICAP’s senior technical director, is quoted in a May 12 Bloomberg article on the possible long-term effects of COVID-19 infection.
“There is such a wide range in the way the illness affects people. The various stakeholders need solid data to help them understand the breadth and duration of long term effects,” said Jessica Justman, a professor of medicine in epidemiology at Columbia University.
May 11: New Scientist interviewed Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, for a May 11 article on the easing of COVID-19 lockdowns in some African countries:
Ultimately, lockdowns are tough for vulnerable people in both South Africa and Ghana, says El-Sadr, and governments must look to provide food packages and income support. “If this does not happen, many will suffer and it will compel people to break lockdown measures in order to survive,” she says.
May 8: During a Columbia Center for the Study of Social Difference event on May 8, 2020, Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, gave a presentation on the important role nurses play during public health emergencies, sharing her experiences as a nurse during both the HIV/AIDS pandemic and the 2014 Ebola epidemic. She introduced a recorded oral history from her colleague James Harries, a registered nurse working on the front lines of the COVID-19 pandemic in Liberia, saying:
“[During the HIV epidemic], I saw the power of nurses and nursing as we cared for the sick and dying without any treatment and limited infection control equipment. I thought those days had passed. Amidst the COVID-19 pandemic, the voice of Harries takes on a special significance as history repeats itself. As the wisdom, lessons, and voices of nurses continue to go unheeded, experiences like Harries’ are being repeated across the globe.”
Also on May 8, Dr. Michaels-Strasser gave a presentation at an Association of Nurses in AIDS Care virtual meeting on the important role HIV nurses can play during public health emergencies. She shared anecdotes from her time working as a nurse on the front lines of the HIV/AIDS pandemic in sub-Saharan Africa as well as her advocacy work today for nurses on the front lines of the COVID-19 pandemic.
“Many nurses around the world don’t have the environmental or administrative controls to keep themselves safe and their patients safe. Now is the time to speak up as nurses, to speak truth to power, to ensure that we have important training in personal protection measures…There is no vaccine for COVID-19 yet, but until that time, we must safeguard our health workers.”
May 7: Al Jazeera interviewed Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, for a May 7 article on the risks of loosening lockdowns while the COVID-19 pandemic continues.
Wafaa El-Sadr, professor of epidemiology at Columbia University, said easing curbs in some states while the US remained in the grip of the pandemic was a “risk and a gamble” as “epidemics don’t know borders”.
“A major Achilles heel for many states in the US is the availability of sufficient testing capability,” she said. “Another challenge is the urgent need for a large cadre of health workers poised to do the hard work of going out into communities to expand testing, do case and contract tracing.”
Also on May 7, Chinese outlet CGTN.com spoke to Jessica Justman, MD, ICAP’s senior technical director, in a video interview on the development of a COVID-19 vaccine.
CGTN spoke to Jessica Justman, ICAP’s senior technical director at the Columbia University Medical Center. She didn’t believe that is will possible to have a vaccine that’s really ready to go by end of this year.
She said, “As much as we want everybody to go quickly, we also want everybody to be careful and develop a vaccine that is both safe and truly effective. There’s no point vaccinating people with something that will be harmful.”
She also encourages everyone to wear masks. “So to think carefully before you take risks and expose yourself to others and to remember that the mask is about protecting other people, not about protecting yourself,” She said.
May 6: ICAP is one of the CDC implementing partners in Zimbabwe that will manage a funding package of $3 million to strengthen local health systems to respond effectively to COVID-19.
CDC awarded the new funding through existing CDC Zimbabwe implementing partners, ICAP at Columbia University, the Biomedical Research and Training Institute and the International Training and Education Centre for Health.
They said the fund was meant to increase laboratory diagnostic capacity, enhance central and district-level surveillance, strengthen infection, prevention, and control in healthcare facilities and support vaccine preparedness.
CDC will also use approximately US$75 000, part of the US$150 000 previously announced President’s Emergency Plan for Aids Relief (Pepfar) funds, to support COVID-19 prevention measures for people living with HIV.
May 5: Jessica Justman, MD, ICAP’s senior technical director, returned to WNYC’s Brian Lehrer Show on May 5 to discuss how COVID-19 spreads.
“I think it’s important to remind ourselves that the reason we wear masks is not to protect ourselves from breathing in air from other people, it’s to protect others from breathing in our air in case we have the infection in its very early stage and we don’t realize that we might be transmitting it. I know it ‘s counterintuitive, we want to believe that when we put on a mask we’re protecting ourselves, but it really is about protecting other people.”
Also on May 5, Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, was interviewed in an article in The Hill about opening national parks and the potential impact on the COVID-19 epidemic in the U.S.
Meanwhile, Michaels-Strasser from Columbia said that reopening the parks too early could make the virus harder to track because waves of out-of-state visitors to national parks will complicate contact tracing because every state has its own system.
“The complexity of it increases exponentially,” she said. “You’re dealing with multiple departments, multiple agencies. Connecting the dots just gets harder and harder the more movement that is happening.”
Additionally, Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, presented on “COVID-19: Where Are We and Where Are We Going?” during a May 5 webinar hosted by the TRAIN Learning Network.
May 4: Columbia Magazine interviewed Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, as part of its Spring/Summer 2020 cover story, “What We Have Learned From the Pandemic (So Far).” The interview was published on the Columbia Magazine website on May 4.
ICAP has identified lessons from HIV and Ebola that could streamline governments’ response to COVID-19.
“First,” says El-Sadr, “governments must gain the trust of their populations. They must be transparent and communicate frequently in order to prevent rumors and conspiracy theories.” Misinformation plagued the response to HIV and Ebola, leading many people to dismiss the threats or see them as government plots. And fears of being stigmatized prevented the sick from getting help. “You must mobilize opinion leaders to assuage these anxieties. We learned how to do that effectively for HIV, and we will now have to apply those lessons to a much more transmissible virus.”
Also on May 4, ICAP’s Yen Pottinger, PhD, Senior Lab Advisor, spoke at a virtual edition of the Ambassador William C. Battle Symposium on American Diplomacy, hosted by the Miller Center at the University of Virginia. This year’s symposium took an in-depth look at U.S.–Chinese relations during the coronavirus pandemic.
“We saw in the early days that China was very forthcoming with their data, and this was extremely important…The countries where viruses begin have a special responsibility to share data early, unfiltered to the global community so that people can prepare for when the virus hits their shores.”
May 1: Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, is quoted in a May 1 National Geographic article on lessons learned from national responses to the COVID-19 pandemic.
However, lessons from one country aren’t necessarily applicable to another. For example, New Zealand announced earlier this week that it has effectively eliminated the virus from its shores, “but it might not have attributes that would fit with New York City or many densely populated parts of the U.S. and Europe,” says Wafaa El-Sadr, an epidemiologist and director of ICAP at Columbia University, an initiative that strengthens health systems in resource-poor countries.
April 29: Chinese outlet Interface News interviewed Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, for an April 29 article on the U.S. COVID-19 response in the three months since the total number of cases globally passed the one-million mark.
Although there is a point that the antibody test is used to screen immune populations on a large scale, El-Sadr pointed out to Interface News: “It is too early (to judge the role of the antibody test). It is not known what proportion of humans produce antibodies after being infected with the new coronavirus, it is not yet known how long these antibodies will last, and it is not known whether these antibodies provide lasting immunity.”
April 28: Jessica Justman, MD, ICAP’s senior technical director, spoke on MSNBC’s “All In with Chris Hayes” on April 28 about the process currently underway for developing a vaccine that could prevent COVID-19.
“This is a strategy of using a virus that is very common, called adenovirus, which can cause a common cold. They make it so it can’t really replicate, and they engineer it so that it has genetic material from another virus inside, like a Trojan horse vaccine. Once it’s inside, the proteins that are going to be synthesized by the genes inside that virus can develop an immune reaction. They’ve been working on this strategy for 20 years, and they have safety data from a MERS vaccine they worked on in the past year, so that allows them to move forward more quickly. I will say that I think their timeline is extremely ambitious. I hope, just like everybody else, that they’re right, and that they can move this quickly.”
Also on April 28, Al Jazeera quoted Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, on missed opportunities to strengthen the U.S. public health system that could have greatly lessened the impact of the ongoing COVID-19 pandemic.
“There were numerous missed opportunities in the long term investing of public health. The budgets for public health have been significantly decreased over the years and this whittling away of our public health system has really weakened our ability to respond.”
April 26: NPR affiliate KUOW spoke to Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, for an April 26 Q&A on how health systems in low- and middle-income countries (LMIC) can adapt strategies to fight COVID-19 given limited resources:
For low-income countries that struggle with weak health systems, large populations of impoverished people and crowded megacities, “there needs to be a very major adaptation” to the established measures we’ve been using to fight COVID-19, says Dr. Wafaa El-Sadr, an epidemiologist and director of ICAP, a global health organization at Columbia University.
“I think they’re trying, but it’s not easy,” El-Sadr says. “Ministries of health are working, partnering with international organizations to try to innovate — and hopefully, if the innovation works, it can be scaled up.”
April 25: Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, is quoted in an April 25 article in Indian outlet The Print examining why South Asia is experiencing lower COVID-19 infection rates than other areas of the world:
“The way respiratory viruses like the novel coronavirus are transmitted in various regions does not differ,” said Wafaa El-Sadr, director and professor of epidemiology and medicine, Columbia University, New York. Around the world, observations and studies have unanimously indicated that the virus is primarily spread through respiratory droplets containing the virus, as well as through close contact with carriers.
“We cannot depend on herd immunity through continued transmission as this novel coronavirus has a high mortality rate, almost ten times higher than mortality from seasonal influenza,” El-Sadr added.
Dr. El-Sadr is also quoted in an April 25 article in IndiaSpend covering the recent launch of the World Health Organization (WHO) “Access to COVID-19 Tools (ACT) Accelerator” to hasten the development, production, and equitable access to essential COVID-19 health technologies.
“It is important that countries in Asia and Africa anticipate that a vaccine will hopefully become available within a year or a year and half and do everything possible to make it possible to get these vaccines to the people who need them as soon as possible,” Wafaa El-Sadr, director of ICAP at Columbia University and professor of Epidemiology and Medicine at Columbia’s Mailman School of Public Health told IndiaSpend. Vaccines’ prices must be negotiated so that the global community as a whole can benefit from them, she said.
April 23: Announced on April 23, Jessica Justman, MD, ICAP’s senior technical director, is part of an interdisciplinary study team investigating whether blood plasma from COVID-19 survivors can be used to prevent infections in unexposed healthcare workers and first responders, high-risk individuals, and close contacts of COVID-19 patients, and whether it can treat COVID-19 patients with severe disease.
The study is being led by W. Ian Lipkin, MD, and includes investigators Thomas Briese, PhD, and Nischay Mishra, PhD, of the Columbia Mailman School; Andrew Eisenberger, MD, Eldad Hod, MD, Max O’Donnell, MD, and Steve Spitalnik, MD, of the Columbia University Irving Medical Center; and Beth Shaz, MD, of the New York Blood Center.
“We appreciate the FDA’s approval of this trial, which has the potential to help us protect courageous frontline healthcare workers and first responders during this crisis,” says Lipkin. “Plasma therapy is a long-established approach, developed by Paul Ehrlich and Emil von Behring for treatment of diphtheria and recognized in 1901 by the first Nobel Prize in Physiology or Medicine. Just as COVID-19 has taken us back to classic methods for outbreak containment like isolation, through a novel use we are rediscovering the lifesaving potential of a classic strategy like plasma therapy.”
Also on April 23, ICAP hosted a Grand Rounds Webinar on coronavirus testing with Yen Pottinger and Sam Sia. The recording is available in the Tools & Resources section of the ICAP website.
April 22: ICAP co-hosted a webinar titled “Africa: Confronting COVID-19” in partnership with the Columbia Global Centers in Nairobi and Tunis.
ACCESS THE RECORDING (YouTube)
VIEW SLIDES (ICAP Tools & Resources)
An April 22 MarketWatch article quotes Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, on the power of testing and contact tracing for epidemic control in the face of COVID-19.
Had [contact tracing] been started at the beginning of the outbreak, “we may have been able to get ahead of the transmission of this virus and stop it,” said Dr. Susan Michaels-Strasser, assistant professor of epidemiology at Columbia’s Mailman School of Public Health.
“When widespread community transmission started to occur and new cases started popping up in many locations at once, testing and tracing became unwieldy,” Michaels-Strasser said. “As the curve flattens and goes down and the number of new cases decreases, we need to go back to this action. It is the gold standard in containment of an epidemic.”
April 21: Jessica Justman, MD, ICAP’s senior technical director, is featured in an April 21 Rolling Stone article on COVID-19 immunity, antibody tests, and whether the benefits of immunity certification outweigh the potential consequences.
And yet, even if immunity cards do emerge as the best way forward, there’s a lot to consider. Justman points to the yellow fever immunization cards given to people in Africa who have been vaccinated against the disease as a potential model for immunity cards in the U.S. “For crossing borders, I could imagine some kind of immunity card,” she says. But Justman stresses that it’s important that we look at the other end of the spectrum too — like whether immunity cards would be required in order to go into a grocery store. “That would be too much,” she says, noting that she’s unsure how U.S. citizens would react to having to show a document to be allowed into a supermarket.
Chinese news outlet ECNS interviewed Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP, in an April 21 article on the need for continued international coordination against the COVID-19 pandemic.
Wafaa El-Sadr, a professor of epidemiology and medicine at Columbia University in the United States, said the global outbreak is affecting various parts of the world in different ways. While it is unclear how much longer it will run, it will last “probably in some manner or another until we discover an effective vaccine”, she said.
“Countries around the world are in very different phases of the epidemic. There are certainly places like Europe and the US where the number of cases continues to rapidly increase, while it appears to have stabilized in other parts, including several Asian countries,” El-Sadr said.
Dr. El-Sadr is also quoted in an April 22 Global Times article on the disparate impact of the COVID-19 pandemic along racial and ethnic lines.
Data from the US show there are differences in the infection rate among different racial and ethnic groups. In New York City there is a significantly higher infection noted among Latinos and African Americans, Professor Wafaa El-Sadr at the Epidemiology and Medicine at Columbia University, told the Global Times on Monday.
The difference in infection rates may be due to several reasons, she said. It might be due to the fact that such individuals are more likely to be exposed to cases of COVID-19 through use of mass transit or due to living in more crowded conditions with higher risk of transmission among household members.
April 20: Foreign Policy’s “Don’t Touch Your Face” podcast welcomed Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP, as a guest on its April 20 episode about what needs to be done before the COVID-19 lockdowns are lifted.
“There’s the need to be building an infrastructure and a capability to be able to respond and continue to respond to this epidemic moving forward. One of the ways of being prepared to respond is to increase the capacity for testing. The numbers we see are the numbers of confirmed cases. In many parts of the world, it is only people who are quite sick that are getting the opportunity to get tested. Having the capacity to test more people and loosening up the requirements for testing will be very important. The public health capacity to be able to mobilize and track every case, to do contact tracing, and to make sure that people who are infected or their contacts are able to be isolated or quarantined over time.”
April 19: Tunisian news outlet La Presse interviewed Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP, in an April 19 Q&A.
How long do you think it would take for life to return to normal?
The return to normal depends entirely on the effectiveness of a country in controlling the epidemic on its territory. If the number of cases is brought under control quickly, this would make it possible to soften the recommendations for social distancing and confinement. Therefore, any decision to return to normal will depend on the data of the country and which should be accompanied by rigorous control measures.
April 17: In a New England Journal of Medicine “Perspective” published April 17, Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP at Columbia University, and Jessica Justman, MD, ICAP’s senior technical director, urge a coordinated global effort in the face of the COVID-19 pandemic, with “countries around the world [taking] concrete steps to assist Africa in staying ahead of the curve, even as they confront their own epidemics.”
“When HIV spread like wildfire across the African continent, it took decades for the world to mobilize a response. […] Epidemics know no borders, and success in controlling the epidemic in any one country will be limited if epidemics continue to rage elsewhere. Today, we have the chance to avoid a repeat of history. Africans are doing their part. Now is the time for us to do ours.”
This article was shared via EurekAlert! and is the basis of articles in the Milwaukee Journal Sentinel and Health 24
April 16: Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, spoke on Al Jazeera English’s “Inside Story” about the conditions necessary for countries to start lifting their COVID-19 lockdown measures.
[Any] decision regarding loosening of any of these lockdown measures should be anchored in evidence, it should be anchored in data that are available for each of the countries, and even better for each of the communities that we’re talking about. For example, we need to have evidence that there’s a sustained decrease in the numbers of new infections, and by sustained I mean not just for one day or two days or three days, preferably we need to see that the sustained decrease for ten or fourteen days at a minimum. We need to see also a decrease in the numbers of deaths, and that also should be sustained. And we also need to make sure that we have the resources be able to continue to test people, to identify cases rapidly, and to be able to contain and isolate those cases and their contacts.
April 13: Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, joined a panel of Columbia University experts on April 13 to discuss COVID-19. The session was hosted by University Life and the recording is available on their website.
Panelists included:
- Wafaa El-Sadr, MD, University Professor of Epidemiology and Medicine, Director of ICAP at Columbia University, and Dr. Mathilde Krim-amfAR Chair of Global Health
- Melanie Bernitz, MD, Associate Vice President and Medical Director of Columbia Health
- Scott Hammer, MD, Harold C. Neu Professor of Infectious Diseases and Professor of Epidemiology at Columbia University Irving Medical Center
The event was moderated by Suzanne B. Goldberg, Executive Vice President for University Life.
Also on April 13, Dr. El-Sadr joined a panel of experts to discuss COVID-19 in Africa. The session was hosted by the Center for Strategic & International Studies (CSIS) and the recording is available on their website.
Panelists included:
- Jakkie Cilliers
Chairman of the Board of Trustees and Head of the African Futures and Innovation, Institute for Security Studies - Marius Oosthuizen
Faculty at the Gordon Institute of Business Science, University of Pretoria - Wafaa El-Sadr
University Professor and Dr. Mathilde Krim-amfAR Chair of Global Health, Columbia University
The event was moderated by Judd Devermont, Director of the CSIS Africa Program.
Jessica Justman, MD, ICAP’s senior technical director, is quoted in an April 13 New York Times article on shared quarantine as a practice among families during the COVID-19 pandemic.
With shelter-in-place orders and social distancing rules, some might consider the decision for multiple families to live together or share child-care duties to be unsafe. However, “this kind of arrangement sounds fine,” said Dr. Jessica Justman, the senior technical director of ICAP at Columbia University Mailman School of Public Health, as long as it “means the group is practicing social distancing from all others who are not part of the extended household and everyone in the extended household is truly staying away from all others, and very careful when food shopping, et cetera.”
In an April 13 Q&A with Indian magazine Outlook, Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP, comments on the U.S. and Chinese responses to the COVID-19 pandemic:
It will be critically important to be able to look back, once this pandemic is behind us, to examine the U.S. response in detail, what worked, what did not work and why. In the midst of the outbreak with a rapidly evolving response, it is too early to dissect the various steps taken. Most experts would say that the U.S. took an incremental approach rather than a decisive approach and that may have been the Achilles’ heel.
“Most experts would say that the US took an incremental rather than a decisive approach and that may have been its Achilles’ heel,” says Wafaa El-Sadr, Professor of Epidemiology and Medicine at @Columbia. @ICAP_ColumbiaU#CoronavirusPandemic #COVID2019https://t.co/fcsAsCXct1
— Outlook Magazine (@Outlookindia) April 13, 2020
ICAP’s Andrea Low, MD, PhD, HIV clinical and scientific director for the PHIA Project, spoke with Radio Tunis Chaîne Internationale (RTCI) in an April 13 interview about the COVID-19 pandemic (audio in French):
Dr. Andrea Low (@ICAP_ColumbiaU) was on RTCI this morning to talk about #COVID19. CGC Tunis is proud to partner with Tunisian media outlets to bring Columbia experts and expertise to a wider audience. https://t.co/ZlIKdZe0oL
— CGC | Tunis (@CGCTunis) April 13, 2020
Tunisia’s Express FM radio station also interviewed Dr. Low on April 13 about the COVID-19 pandemic (audio in French):
April 7: On the April 7 broadcast of MSNBC’s Live with Katy Tur, Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, shared her observations of the novel coronavirus’ impact on the U.S. Health Care system:
We weren’t ready. We were caught off guard. We don’t have the infrastructure. We don’t have the surge capacity of the equipment, of the personal protective equipment, of ventilators, of staff, and for our country… …It took way too long everywhere to really wake up and say, we have a very big problem on our hands. And now, thankfully, the American public gets it and they are responding amazingly. Here in New York, I’ve never seen it like this. It’s incredible what people are doing to really protect themselves, but more importantly, protect others and those at risk.
Also on April 7, Dr. Michaels-Strasser spoke to Al-Jazeera English on the importance of protecting health workers on the front lines of the COVID-19 response:
We really have to safeguard our health workers. This is going to be a marathon, not a sprint, and we have to protect them as best we can.
In an April 7 article on Spanish outlet Expansión, ICAP deputy director of strategic information María Lahuerta, PhD, MPH, outlines the steps toward returning to normal from COVID-19:
La epidemióloga Mª Lahuerta del @ICAP_ColumbiaU en @expansioncom “Es igual de prioritario contener la infección cómo proteger al personal sanitario” pic.twitter.com/ETRxdFsuzc
— Irene Tato (@itato) April 6, 2020
Dr. Lahuerta also spoke to Spanish station Telecinco on April 7, explaining that COVID-19 prevention practices such as wearing a mask, washing hands, and keeping social distance must be maintained to avoid infections and, above all, protect at-risk groups.
Viewing the data, she is encouraged but points out that what we need now are “many quick and accessible tests for everyone”, on the one hand those that detect the virus and on the other those that detect the antibodies that are generated once [a person recovers from] the disease. (translation via Google Translate)
Jessica Justman, MD, ICAP’s senior technical director, commented to NY1 on April 7 about socioeconomic factors in preventing and responding to COVID-19:
“Social distancing is a privilege that not everybody has equal ability to practice,” said Dr. Jessica Justman, an infectious disease specialist at Columbia University.
April 6: On April 6, Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP, spoke on Kenyan network Citizen TV’s “Daybreak” program:
“My word is to take this very seriously… take the prevention methods to heart and practice them and try to observe the population measures and the social distancing measures…” – Dr. Wafaa EL- Sadr, Director of ICAP at Columbia University#DayBreak@SamGituku pic.twitter.com/QoEZdzK8uh
— Citizen TV Kenya (@citizentvkenya) April 7, 2020
April 3: On April 3, Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP, answered questions about COVID-19 on the live CSPAN program Washington Journal.
“I think there are lots of lessons learned. One that is very important is putting in place strong and universal mitigation measures. As difficult as it can be for people to completely change their social behavior, they are vital. They are really the one things we have at our fingertips to enable us to control the epidemic.”
April 2: The Atlantic reached out to Jessica Justman, MD, ICAP’s senior technical director, for an article on best practices for quarantining with roommates.
Experts say there are best practices to follow. Don’t share hand towels with roommates, and regularly disinfect often-used surfaces like counters, faucets, remotes, and refrigerator handles, Jessica Justman, an epidemiology professor at the Columbia University Mailman School of Public Health, told me. When you’re moving from a communal space to another room, wash your hands. “Wash your hands more times than you think would be possible.”
Dr. Justman is also quoted in a Guardian article on the effectiveness of facemasks for preventing the spread of COVID-19:
It’s like a pitcher and a catcher at a baseball game. And the masks are all about trying to keep the pitcher from pitching the ball. There are more pitchers than we realized, and if we need to all wear masks in order to keep the pitchers from pitching their balls, then so be it.
In an April 2 article in Spanish outlet El País, Dr. Justman explained how job and housing situations for working-class individuals and families in New York City increase the likelihood of COVID-19 exposure and infection:
Various factors may weigh on the different incidence, such as the number of tests that are performed, although Dr. Jessica Justman, an epidemiologist and infectious disease specialist at [ICAP at Columbia University], highlights the sociological factor. “It makes sense that working-class areas suffer more exposure to the virus, their jobs in essential services, shops, etc., have not closed, as also happens with health personnel, and they move more; they also tend to share housing more frequently,” she points out. (translation via Google Translate)
Also on April 2, ICAP hosted a Grand Rounds webinar on social distancing with Melanie Bernitz. The recording is available in the Tools & Resources section of the ICAP website.
April 1: Jessica Justman, MD, ICAP’s senior technical director, is quoted in a New York Times article showing how the COVID-19 epidemic in New York City is hitting low-income neighborhoods the hardest.
Dr. Jessica Justman, an epidemiologist at Columbia University in Manhattan, said the numbers were most likely because many immigrants and low-income residents live with large families in small apartments and cannot isolate at home. “I think unfortunately this is showing how devastating that can be,” Dr. Justman said.
March 31: Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director for human resources for health, advocates for the protection of nurses and other frontline health workers in an op-ed published in The Hill, sharing her lessons learned from her work during the 2014 Ebola outbreak in West Africa.
Our failure to prepare and implement the lessons learned from the Ebola outbreak could very well sentence our nurses to the same fate. Our health workers are critical to controlling this pandemic and we must do our utmost to keep them safe now — and when it happens again.
March 28: In a March 28 article in Xinhua, Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP, welcomed increased scientific collaboration between the U.S. and China in the face of the COVID-19 pandemic:
Wafaa El-Sadr, director of the Global Health Initiative and ICAP at Columbia University’s Mailman School of Public Health, said “this virus does not discriminate, and we are all vulnerable.” The seasoned expert said that by strengthening collaboration on various fronts such as scientific research, China and the United States can contribute to the tackling of major global public health threats. “This is the time to build bridges, not walls, between peoples around the world,” said El-Sadr, adding she was “encouraged to see the sharing of information and scientific data across borders,” which is “critical” in working towards controlling this pandemic.
Dr. El-Sadr also spoke on Chinese network CCTV:
“Our current understanding of the virus is based on the experience of China … we have learned a lot through the study of Chinese data.”
Jessica Justman, MD, ICAP’s senior technical director, spoke on Uptown Radio about New York City’s pilot plan to close sections of streets in order to create more space for people to be outside while still practicing social distancing.
“I think the city’s pilot plan to close certain sections of certain streets to get more open space is a really great idea. I had heard that Central Park and other parks have become very crowded, and I think we can anticipate that will only increase as the weather becomes warmer. Creating more open space for people to go outside but still have enough space to practice social distancing is a terrific idea.”
March 27: Jessica Justman, MD, ICAP’s senior technical director, offers advice for maintaining social distance while grocery shopping in a March 27 article in TIME.
Many national chains have announced precautions they’ll be taking moving forward, and you can also call your local store and ask ahead before you leave the house. “You want to pick a store that’s really paying attention and making it safer for customers to go in,” Justman says.
March 26: TIME Magazine asked Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, about the need for more health care workers to care for the increased number of critically ill patients during the COVID-19 pandemic:
Data shows hospitals and health centers are reaching their maximum capacity, she explains. “Not only do we have more patients, we have more critically ill patients so it requires a higher level of care,” Michaels-Strasser says. “One nurse can’t take four people; they (often) have to take care of one person because it’s a life or death situation.” Neither expert recalls the U.S. taking such drastic steps in response to a previous infectious disease outbreak, although Michaels-Strasser notes that using back-up doctors and nurses in Sierra Leone during the Ebola outbreak was “done effectively.”
March 25: Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, is featured in a New Yorker article tracing the arc of the COVID-19 epidemic in China.
“Within three days, they had scientists who were able to sequence and characterize the structure of the virus, which is unheard of,” Wafaa El-Sadr, the director of ICAP, a global health center at Columbia University, told me. She said that recent advances in technology made the sequencing possible, a crucial step that allowed scientists to develop ways to diagnose the disease and to start to identify methods of treatment.
Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, joined a panel of Columbia University experts on March 25 to discuss COVID-19. The session was hosted by University Life and the recording is available on their website. Panelists included:
- Wafaa El-Sadr, MD, University Professor of Epidemiology and Medicine, Director of ICAP at Columbia University, and Dr. Mathilde Krim-amfAR Chair of Global Health
- Scott Hammer, MD, Harold C. Neu Professor of Infectious Diseases and Professor of Epidemiology at Columbia University Irving Medical Center
- Lourival Baptista-Neto, MD, Associate Professor of Psychiatry and Vice-Chair of Clinical Services in the Department of Psychiatry at Columbia University Irving Medical Center
- Melanie Bernitz, MD, Associate Vice President and Medical Director of Columbia Health
The event was moderated by Suzanne B. Goldberg, Executive Vice President for University Life. View the recording on the University Life website Watch the recording on YouTube In a March 25 article from Pro Publica, Jessica Justman, MD, ICAP’s senior technical director, says providing detailed geographical information on COVID-19 hotspots may increase the risk of bias attacks and stigma against Asian Americans:
But some of those same factors, particularly ethnicity and race, may account for the city’s reluctance to make public more localized data that could point to clusters in particular neighborhoods, among certain communities. Around the country, there have been disturbing reports of bias attacks against Asian Americans by assailants blaming Chinese communities for the spread of the virus. “The risk is that certain communities would be unfairly stigmatized, especially if communities with many COVID-19 cases already shoulder poverty or high crime,” said Dr. Jessica Justman, associate professor of medicine in epidemiology at Columbia University. “On the other hand, communication and information are always important and especially important in a pandemic setting.”
In a MarketWatch article from March 25, Jessica Justman, MD, ICAP’s senior technical director, notes that population density and income level impact the spread of COVID-19 in New York City:
There’s another aspect to population density that made poorer New York City neighborhoods particularly susceptible, said Jessica Justman, an associate professor of medicine in epidemiology at Columbia Mailman School of Public Health. “It is also about the average number of people living in a household. People living alone in an apartment will be able to practice social distancing more easily than people who live with a large family, or who are sharing space with many others,” Justman said. Household density explains why Queens is the hardest hit borough in the city, as it has a relatively larger population of low-income immigrant families living in greater numbers in smaller spaces, she said. “It makes sense that the epidemic would concentrate in areas where many people occupy the same household,” she said.
March 24: Columbia Public Health Now Podcast host Maria Andriella O’Brien, deputy chief of staff at the Mailman School of Public Health, interviewed ICAP global director Wafaa El-Sadr, MD, MPH, MPA, about how health systems are—or are not—handling the COVID-19 outbreak.
“Initially when there are a few cases, then the public health workforce seeks how to find those cases, quickly identify who has the disease, quickly isolate them, and then of course quarantine their contacts. You can do that while the numbers remain small,” Dr. El-Sadr said. “At the same time, what happens is that the large number of cases overwhelms the public health workforce, and that’s when you need to go to more of the social distancing kind of interventions, for example asking people not to congregate and avoid crowded spaces.”
Listen to the March 24 episode on SoundCloud Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, spoke with Ian Masters on March 24 about the selfless dedication of nurses and the risks they take working in intimate contact with their infected patients. Listen to the episode on SoundCloud Segment with Dr. Michaels-Strasser runs from 22:52 – 42:17.
March 23: Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, and Jessica Justman, MD, senior technical director, published an op-ed in Columbia News on March 23 noting that “Africa is facing the real possibility of a continent-wide tragedy” and calling for action to “enhance preparedness and to stand in solidarity with these most vulnerable countries in our global community.”
For many low and middle-income sub-Saharan African countries, the health system infrastructure remains fragile and ill-prepared for a massive increase in the number of cases. Kenya, with a population of 50 million people, has only 200 intensive care beds in the entire country. For context, the United States, which is on the verge of being overwhelmed by the epidemic in some locations, has 34 intensive care beds for every 100,000 people.
On the March 23 episode of MSNBC’s Hardball, Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, advised audiences to follow the guidance of public health experts:
“Right now the most important thing is protecting our health workers, who are begging for protective equipment, and helping our elderly to stay at home, and for all of us to do what we should do as citizens: stay home, listen to the guidance of Dr. Fauci and Dr. Birx. They know what they are doing, they are data-driven, they are using science to protect all of us, and they are the experts in this regard.”
COVID-19 quarantine measures are expected to last an average of six weeks from the outbreak in each country, and it will probably take at least 12 months for the vaccine, according to Juliana Soares Linn, MD, MPH, MSc, deputy director of disease prevention at ICAP, in a March 23 Q&A for Greek outlet Kathimerini.
“Since February 10, two weeks after the outbreak, fewer than 1,000 cases have been reported per day, and less than 50 cases have been reported since March 7. Today, March 20, China has not reported any new domestic coronavirus infections. Assuming the U.S. and other countries apply a similar response, social distancing will be mandated until the incidence is reduced to less than 1,000 per day and then recommended until there are less than 100 cases per day. With reference to the timetable of the epidemic in China, this means six weeks after the peak, which may vary by country.” Translation via Google Translate
March 22: In a March 22 AP article, Jessica Justman, MD, ICAP’s senior technical director, advises readers to visit the CDC and WHO websites for the most reliable information about COVID-19:
Dr. Jessica Justman, an infectious disease expert at Columbia University, said the sheer amount of information online about the coronavirus pandemic can quickly become overwhelming. That’s one reason she encourages people to check the websites of the CDC and the WHO. “It’s not just misinformation, it’s also a lack of good information,” Justman said. “There’s so much information out there that many people are just saying ‘I can’t read it, it makes me too anxious.’” “Go straight to the source,” she said. “The CDC has been putting out great information.”
March 19: The Columbia Daily Spectator asked Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, about how Columbia University’s housing resources are being shifted from student use to care for patients with COVID-19.
University Professor Wafaa El-Sadr, director of the Global Health Initiative at the Mailman School of Public Health, believes that within the next few months we will have a better sense of the trajectory of the outbreak. Until then, however, it is vital that various entities continue to plan ahead. “One of the most important things to think about is, ‘What is the capacity?’” said El-Sadr. “Not just the capacity today of our health system, but to think of what will be needed tomorrow, and next week, and the week after, and so on. I think this is what’s been done elsewhere, to anticipate the need for more space to house people who have COVID-19 and if the need arises, then, to be able to utilize the resources and the capacity that exists in empty housing.”
March 18: A Guardian Q&A panel on intimacy during the COVID-19 outbreak included Jessica Justman, MD, ICAP’s senior technical director and Associate Professor of Medicine in Epidemiology at the Columbia University Mailman School of Public Health.
So is it OK to have sex? Justman: If you or your partner is a Covid-19 case, the advice is to steer clear of each other as much as possible. In fact, the New York City department of health has guidelines on this. If you’re a possible or confirmed case you should isolate yourself, ideally in a private residence until seven days after the illness began. You need to have had no fever for 72 hours, without using ibuprofen [see footnote] or anything that would mask your fever, and your respiratory symptoms should be improving.
On March 18, WNYC’s Brian Lehrer Show welcomed back Jessica Justman, MD, ICAP’s senior technical director, to discuss social distancing.
“The average time to get sick after being exposed is about five days, but it can take as long as 14 days,” said Dr. Justman. “I think a two-week period will allow us to get a better sense of what impact our current social distancing is having on the number of new cases. If it’s working, we should start to see a reduction in the number of new cases in about two weeks from now.”
ICAP’s Yen Pottinger, PhD, senior laboratory advisor for the PHIA Project, joined a PBS “Firing Line” Q&A on Instagram with host Margaret Hoover:
NY City Lens asked Susan Michaels-Strasser, PhD, MPH, RN, FAAN, ICAP’s senior director of human resources for health (HRH) development, about personal protective equipment in light of COVID-19 concerns.
Do we need to wear masks? The answer is no. Most masks that you’ve seen people walking down the street wearing —the blue disposable ones—won’t protect you against viruses, according to Susan Michaels-Strasser, an assistant professor of epidemiology at the Columbia University Medical Center. Particles, she said, will still be able to enter because the masks are loose on the sides and on top. If you do decide to wear a mask, it needs to be a tight fitting N95 mask.
March 17: Newsweek quoted ICAP’s senior technical director, Jessica Justman, MD, in a March 17 article on COVID-19 symptoms and spread.
The new member of the large coronavirus family of pathogens does not appear to infect the body in a particularly unique way, Jessica Justman, associate professor of epidemiology at Columbia University Mailman School of Public Health, told Newsweek. Like other viruses, it binds to a receptor found on many cells in the body, including those in the lower respiratory tract. The microbes, which are a protein coat filled with genetic material, then hijack the cells in order to replicate. This is why some COVID-19 patients develop pneumonia, an infection of the air sacs in one or both lungs, said Justman.
BBC News Brasil quoted Dr. Justman on COVID-19 containment and mitigation measures. In Portuguese:
“Eu acho uma boa ideia (o fechamento de fronteiras). Quanto mais se limitar a mistura de pessoas de uma área geográfica a outra, mais sucesso teremos em retardar a propagação”, diz à BBC News Brasil a especialista em doenças infecciosas Jessica Justman, professora da Columbia University, em Nova York.
In English (courtesy of Google Translate):
“I think it’s a good idea (the closing of borders). The more the mixing of people from one geographical area to another is limited, the more successful we will be in delaying the spread,” infectious disease expert Jessica Justman tells BBC News Brazil, professor at Columbia University in New York.
Dr. Justman is featured in a March 17 MarketWatch article and a March 16 Guardian Q&A about social distancing.
“If we really do a good job with social distancing, and we see the expected impact on the number of new cases, I think that could in turn allow us to begin to ease up,” said Jessica Justman, an infectious-disease expert at Columbia University’s Mailman School of Public Health. If Americans don’t do a good job with social distancing or it doesn’t work as well as expected, the measures would need to be prolonged, she said.
Dr. Justman’s recommendations were also cited in Metro.uk.
March 14: Dr. Justman is featured in a March 14 New York Times article answering questions about travel during the coronavirus pandemic and a March 13 WNYC segment on social distancing. She is also quoted in a March 12 Bloomberg article on how the U.S. and Europe can learn from Asia’s response to the pandemic.
“No matter how your health systems or political systems are organized, the keys to epidemic control remain the same” — test, trace, isolate and inform, said Jessica Justman, a professor of medicine in epidemiology at Columbia University.
March 10: On March 10, Wafaa El-Sadr, MD, MPH, MPA, global director of ICAP, co-hosted a special session at the annual Conference on Retroviruses and Opportunistic Infections. The session, titled “Epidemiology, Virology and Control of COVID-19 (CROI Updates),” featured presentations from Zunyou Wu, MD, John Brooks, MD, Ralph Baric, PhD, and Anthony Fauci, MD.
March 9: On March 9, Susan Michaels-Strasser, PhD, MPH, RN, FAAN, senior director of human resources for health development at ICAP, spoke on two segments on MSNBC. Video of the evening segment is available on the MSNBC site.
Jessica Justman, MD, senior technical director at ICAP, spoke on WNYC’s Brian Lehrer Show in the morning and during an hour-long evening special, “Your Coronavirus Questions Answered.”

March 5: On March 5, Jessica Justman, MD (ICAP at Columbia University) and Wan Yang, PhD (Department of Epidemiology, Mailman School of Public Health) presented on COVID-19 for a special edition of ICAP’s Grand Rounds webinar series. The recording is available here.
February 26: Wafaa El-Sadr, MD, MPH, MPA, ICAP’s Global Director and University Professor of Epidemiology and Medicine at Columbia University, spoke to Chinese news outlet Xinhua in an interview published on February 26. A video of the interview was published February 27. A further article was published February 28. Dr. El-Sadr was also featured in the February 26 “Quotes of the Day” from Xinhua.
“‘It’s very heartening to see how quickly Chinese scientists were able to identify the sequence of the virus’ and published it rapidly thereafter, said Dr. El-Sadr. These are ‘very useful to the global community to understand what this disease looks like.'”

February 25: Dr. Justman is quoted in a February 25 Bloomberg Businessweek article on China’s use of surveillance to track COVID-19 cases and contacts:
“The usefulness of high-tech surveillance tools will be limited until officials identify the incubation period of the new coronavirus and develop rapid diagnostic tests and effective treatment, says Jessica Justman, associate professor of medicine in epidemiology at Columbia University and senior technical director of its global public health center, ICAP. Without a better understanding, ‘it’s going to make it much harder to effectively use the kind of cellphone and other data people are imagining,’ says Justman, who has gone door-to-door across Africa, testing people for HIV to map its spread and provide them with treatment options.”
Dr. Justman is also quoted in a February 15 AFP Q&A about testing for coronavirus in China that appeared across numerous outlets and in Spanish, French, and Portuguese:
“‘It’s a very interesting and logical approach,’ said Jessica Justman, associate professor of medicine in epidemiology at Columbia University, [about Hubei health officials using lung imaging to confirm pneumonia in suspected COVID-19 cases rather than performing an RT-PCR test, which requires special equipment, a clean environment, and highly skilled staff]. Using lung images only works for ‘people with more advanced symptoms,’ she told AFP, which means it would not be used to screen patients early on. But for those later-stage individuals, if there is no access to RT-PCR tests ‘it makes sense.'”
February 14: Dr. El-Sadr moderated a panel to address key questions about COVID-19 on Friday, February 14. Panelists included Robert Fullilove, EdD, Dept. of Sociomedical Sciences; Jessica Justman, MD, ICAP at Columbia University; Julie Kornfeld, PhD, MPH, Vice Dean for Education; Nischay Mishra, PhD, Center for Infection and Immunity; and Wan Yang, PhD, Dept. of Epidemiology. VIEW THE RECORDING 
February 12: Dr. El-Sadr recently sat down with China-based vlogger Jerry Kowal to discuss the coronavirus outbreak. The February 12 video is available on YouTube with Mandarin subtitles (English audio starts at 0:47).
February 5: Columbia University has tapped Dr. El-Sadr’s expertise in infectious disease epidemiology on several recent occasions to address concerns about the novel coronavirus. She joined a panel of Columbia experts for a University Life forum on February 5 and is featured in a Mailman School of Public Health article from February 4. The University of Connecticut Daily Campus covered the panel in an article on their website. READ THE ARTICLE ON THE MAILMAN SCHOOL WEBSITE
For over 15 years, ICAP has strengthened health systems worldwide to address infectious disease epidemics including HIV/AIDS and the Ebola virus.
A global health leader since 2003, ICAP was founded at Columbia University with one overarching goal: to improve the health of families and communities. Together with its partners—ministries of health, large multilaterals, health care providers, and patients—ICAP strives for a world where health is available to all. To date, ICAP has addressed major public health challenges and the needs of local health systems through 6,000 sites across more than 30 countries.