Article and Study Summary:
Point-of-care HIV viral load testing combined with task shifting to improve treatment outcomes (STREAM): Findings from an open-label, non-inferiority, randomised controlled trial
Published in:
Lancet HIV. 2020;7 (4):e229-e237.
https://doi.org/10.1016/S2352-3018(19)30402-3
Authors:
Drain PK, Dorward J, Violette LR, et al.
Summary:
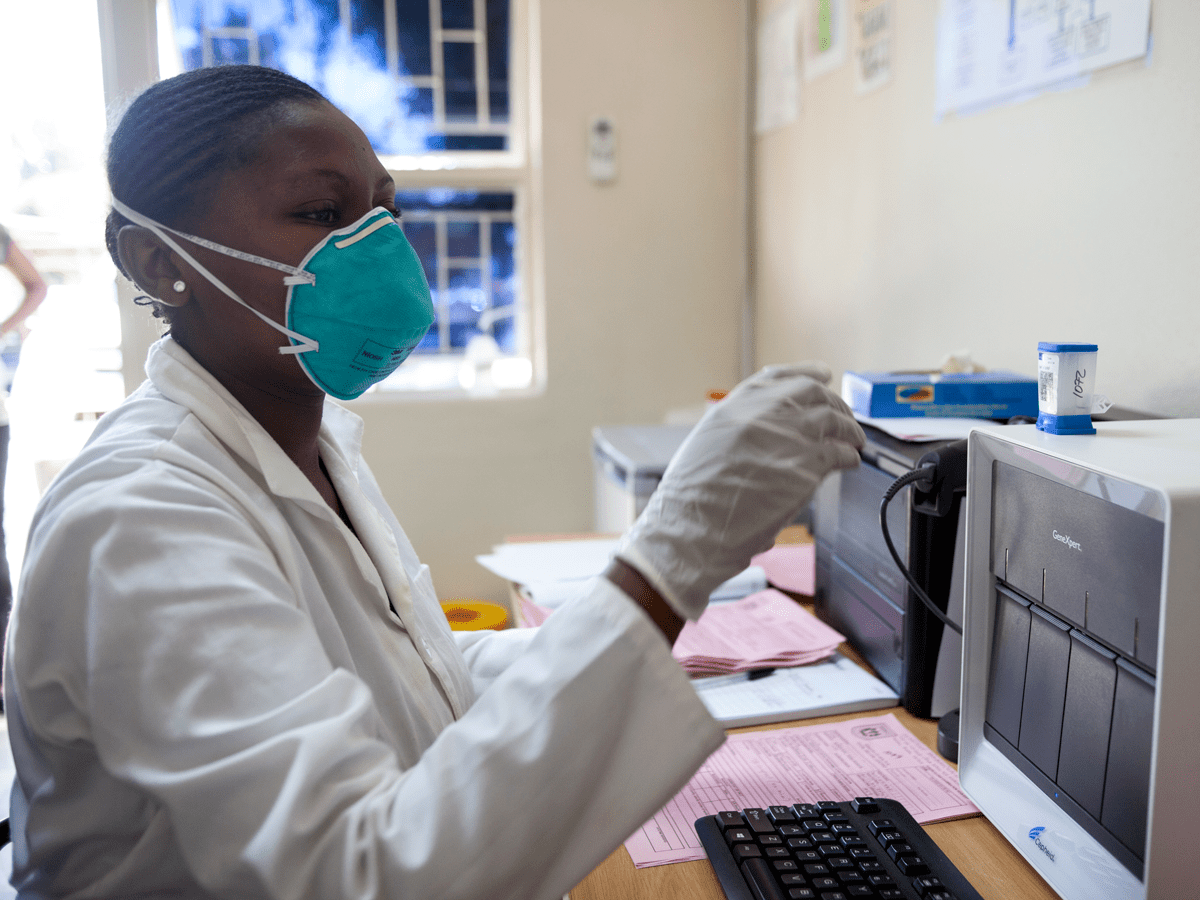
The STREAM study was a single-site, open-label, non-inferiority, randomized controlled trial that evaluated treatment outcomes in people living with HIV (PLHIV) who received point-of-care (POC) HIV viral load (VL) testing, combined with task shifting, in Durban, South Africa. Adult PLHIV receiving routine VL monitoring six months after initiating antiretroviral therapy (ART) were randomized to either an intervention group or a standard of care (SOC) group. The intervention included POC VL testing using Xpert, same-day return of VL results, and task shifting to nursing staff with less formal training. The SOC group received routine HIV care per national guidelines, including laboratory-based VL testing. Participants in the intervention group were found to have significantly better retention in care and VL suppression after 12 months compared to those receiving SOC. Participants in the intervention group were also more likely to receive their VL results, more likely to be enrolled in a community-based ART model, and more likely to be appropriately switched to second-line ART. These findings suggest that POC VL testing, combined with task shifting, is a promising intervention, with multiple potential benefits at the client and program level.
Discussion Questions:
- How could the findings in this study impact VL policy where you work?
- How would these findings be applied in programs you work with? Do you have any experiences to share?
Please share your thoughts and experiences with us in the comments section below.
Full Synopsis:
PDF version available in English, French, and Portuguese
Study Summary
The Simplifying HIV TREAtment and Monitoring (STREAM) study was a single-site, open-label, non-inferiority, randomized controlled trial that compared treatment outcomes in people living with HIV (PLHIV) who received point-of-care (POC) HIV viral load (VL) testing combined with task shifting, to those who received standard-of-care (SOC) laboratory-based VL testing and HIV services.
Study Setting
- A large public clinic that provides HIV and primary care services for more than 10,000 patients in Durban, South Africa.
Methods
- Study participants were PLHIV aged ≥18 years, who presented for their first routine VL test six months after initiation of antiretroviral therapy (ART).
- PLHIV were excluded from the study if they were pregnant, had active tuberculosis, or required acute medical care by a physician at enrollment.
- Participants were randomly assigned (1:1) to either receive POC VL testing with same-day counseling and care provided by an enrolled nurse (intervention group) or laboratory-based VL testing with care provided by a professional nurse (SOC group).
- Enrolled nurses receive two years of training and received additional training in ART management for this study, whereas professional nurses receive four years of training and routinely manage ART in South Africa.
- All routine testing in the intervention group was done onsite using POC technology, including creatinine, CD4 cell count, and HIV-1 VL using Xpert. Participants were asked to wait in the clinic for the results, and POC testing was initiated at the start of the clinical visit to reduce wait times.
- In the intervention group, participants with viral suppression at enrollment and no comorbidities were seen by an enrolled nurse for routine clinical visits. If the enrolled nurse detected abnormal vital signs or clinical symptoms, participants were referred to a professional nurse.
- In the SOC group, participants were seen by a professional nurse and all blood specimens were sent to the National Health Laboratory Service. Per standard practice, participants received their results at their next clinical visit, which was scheduled at the clinician’s discretion and typically occurred after four weeks or eight weeks.
- Sociodemographic and medical information was obtained from participants on enrollment, and all participants were followed for 12 months.
- All participants received HIV care according to national guidelines, which included enhanced adherence counseling for those with a VL >1000 copies/milliliter, switch to second-line ART if their VL remained elevated after two months, and access to a program to collect ART at community pick-up points if eligible.
- Participants were eligible for the community ART program if they were not pregnant, clinically stable, had a VL <40 copies/milliliter at six months and 12 months after ART initiation, and had a CD4 count >200 cells/microliter.
- Once referred, participants collected ART every two months at community pick-up points and were reviewed at the clinic by a professional nurse after six months.
- The primary outcome was a composite measure of retention in care with viral suppression (<200 copies/milliliter) after 12 months. Retention in care was defined as collecting ART at the study clinic or a community pick-up point 44 to 56 weeks after study enrollment.
- Secondary outcomes included viral suppression using thresholds of <1000 and <50 copies/milliliter, time to detection of virological failure and switch to second-line ART, turnaround time of VL results, and participant referral into the community ART program.
Study Population and Follow-up
- Between February and August of 2017, 657 potential participants were screened and 390 were enrolled in the study, with 195 participants assigned to each group.
- The median age of participants was 32 years (interquartile range [IQR] 27–38) and 60% were female. Most participants earned less than 280 USD per month, took public transportation to the clinic, and estimated their travel distance to be more than five kilometers.
- The median CD4 cell count was 468 cells/microliter (IQR 309–666) at study enrollment and 5% had an unsuppressed viral load (>1000 copies/milliliter).
Primary Outcome
- After 12 months of clinical follow-up, 90% of participants in the intervention group and 76% of participants in the SOC group were retained in care with viral suppression (absolute risk difference 13.9%; 95% confidence interval [CI] 6.4–21.2; p<0.00040).
- Each component of the primary outcome was higher in the intervention group than the SOC group, with a 10.3% (95% CI 3.9–16.8; p = 0.0025) higher rate of viral suppression and a 7.7% (95% CI 1.3–14.2; p = 0.026) higher rate of retention in care.
Secondary Outcomes
- The intervention group had significantly higher rates of viral suppression compared to the SOC group, using VL threshold values of <1000 copies/milliliter (absolute risk difference 9.2%; 95% CI 3.2–15.4; p = 0.0041) and <50 copies/milliliter (absolute risk difference 10.3%; 95% CI 2.8–17.6; p = 0.0099).
- All but one of the 398 POC VL results were entered into the health information system on the same day, whereas laboratory-based results were entered and available to clinicians a median of 2 days (IQR 1–4) after blood draw.
- Overall, >99% of POC VL results were communicated to participants by their provider, compared to 82% of results in the SOC group (absolute risk difference 18.3%; 95% CI 14.5–22.5; p<0.0001). Almost all (99%) POC VL results were communicated to participants on the same day, whereas laboratory-based VL results were communicated at participants’ next clinical visit, which were a median of 28 days (IQR 28–54) after the blood draw.
- Seven (4%) participants in the intervention group and nine (5%) in the SOC group developed viral failure. The median time from study enrollment to detection of viral failure was 55 days (IQR 55–57) in the intervention group and 123 days (IQR 98–162) in the SOC group.
- Among six participants with viral failure in the intervention group, 100% were appropriately switched to second-line ART; three participants were switched on the same day, and two participants were switched within one week. Among nine participants with viral failure in the SOC group, four (44%) were appropriately switched to second-line ART a median of 76 days (IQR 20–134) after the second confirmatory VL blood draw (hazard ratio [HR] 10.9; 95% CI 2.1–57.5; p = 0.0050).
- Overall, 59% of participants in the intervention group and 27% in the SOC group were referred into a community-based ART program (HR 3.5; 95% CI 2.5–4.8; p<0.0001).
- Among those referred into the community-based ART program, the median time from study enrollment to referral was 168 days (IQR 168–175) for the intervention group and 261 days (IQR 231–281) for the SOC group.
Critical Analysis
The STREAM study was a single-site, open-label, non-inferiority, randomized controlled trial that found POC VL testing, combined with task shifting, improved retention in care and viral suppression in PLHIV compared to SOC. Those receiving the intervention were also more likely to receive their VL results, more likely to be enrolled in a community-based ART model, and more likely to be appropriately switched to second-line ART.
The following points should be considered when interpreting the study findings:
- This study implemented two interventions at the same time (POC VL and task shifting) and therefore could not evaluate the independent effects that each had on measured outcomes.
- Although this study was an open-label design, analyses were blinded and outcomes were objective measures.
- The study was done in a single, well-resourced, urban site, which may limit generalizability of these findings to other, more diverse settings.
- Use of the Xpert viral load test makes this intervention replicable in settings where Xpert machines are widely available. However, study staff conducted POC testing and associated clinical care at the site, which may not have reflected routine implementation in clinical settings.
- The SOC had a relatively short turnaround time for VL (median 2 days), and results were available to clinicians through an online reporting system. Therefore, the benefits seen with POC VL testing may be even greater in places with a longer turnaround time for laboratory-based VL testing results.
- This study was done before dolutegravir (DTG) was widely available. DTG is expected to improve the rate of viral suppression; therefore, it is unclear if the viral suppression benefits seen in the POC intervention would be as great in the context of widespread DTG use.
- This study enrolled PLHIV six months after starting ART; therefore, findings are not generalizable to PLHIV who are newly initiating ART and it is unclear whether the task-shifting described would be appropriate for this population.
- This study was done before a recent emphasis on Undetectable=Untransmittable (U=U) messaging. Same-day VL results could improve adherence counseling and have psychosocial benefits for patients related to U=U, beyond what is documented in this study.
Implications
The STREAM study was a single-site, open-label, randomized clinical trial that found POC VL testing using Xpert, combined with task shifting, improved retention in care and viral suppression in PLHIV compared to SOC. Other benefits of the intervention included improvement in return of VL results, more timely referrals to less-intensive community ART models, and better recognition and management of treatment failure. These findings suggest that this intervention is a promising approach for monitoring PLHIV on ART, with multiple potential benefits at the client and program level. However, programs will also need to evaluate human resource needs, cost implications, and other logistical challenges before implementing a similar strategy.
This article synopsis was written by Cassia Wells. Share your thoughts on this article or suggest an article for Journal Club by emailing her at caw2208@cumc.columbia.edu
Articles of Note:
- Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
- Compassionate Use of Remdesivir for Patients with Severe Covid-19
- A Trial of Lopinavir–Ritonavir in Adults Hospitalized with Severe Covid-19
- Renin–Angiotensin–Aldosterone System Blockers and the Risk of Covid-19
- Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19