Article and Study Summary
Prednisone for the Prevention of Paradoxical Tuberculosis-Associated IRIS.
Published in:
N Engl J Med. 2018; 379:1915-1925.
DOI: 10.1056/NEJMoa1800762
Authors:
Meintjes G, Stek C, Blumenthal L, et al.
Summary:
This article reports on a randomized, double-blind, placebo-controlled trial that assessed whether prophylactic prednisone at the time of antiretroviral therapy (ART) initiation could reduce the incidence of paradoxical tuberculosis (TB)-associated immune reconstitution inflammatory syndrome (IRIS) among individuals with advanced HIV disease receiving TB treatment in South Africa. HIV-positive adults with a CD4 count ≤100 cells/microliter who were starting ART within 30 days of TB treatment initiation were randomized to receive either four weeks of daily oral prednisone or placebo. The primary end point was the development of TB-associated IRIS within 12 weeks of ART initiation. Participants receiving the prophylactic prednisone regimen were 30% less likely to develop TB-associated IRIS compared to the placebo group, and there was no evidence of an increased risk of severe infections, cancers, or adverse events associated with prednisone use. These results demonstrate that use of prophylactic prednisone can reduce the incidence of TB-associated IRIS after ART initiation in high-risk HIV-positive adults.
Discussion Questions:
- How could the results presented in this article inform clinical practice in the programs that you work with?
- What programmatic challenges do you foresee in implementing the intervention described in this study? Do you have any experiences to share?
Please share your thoughts and experiences with us in the comments section below.
Full Synopsis:
PDF version available in English, French, and Portuguese.
Study Summary
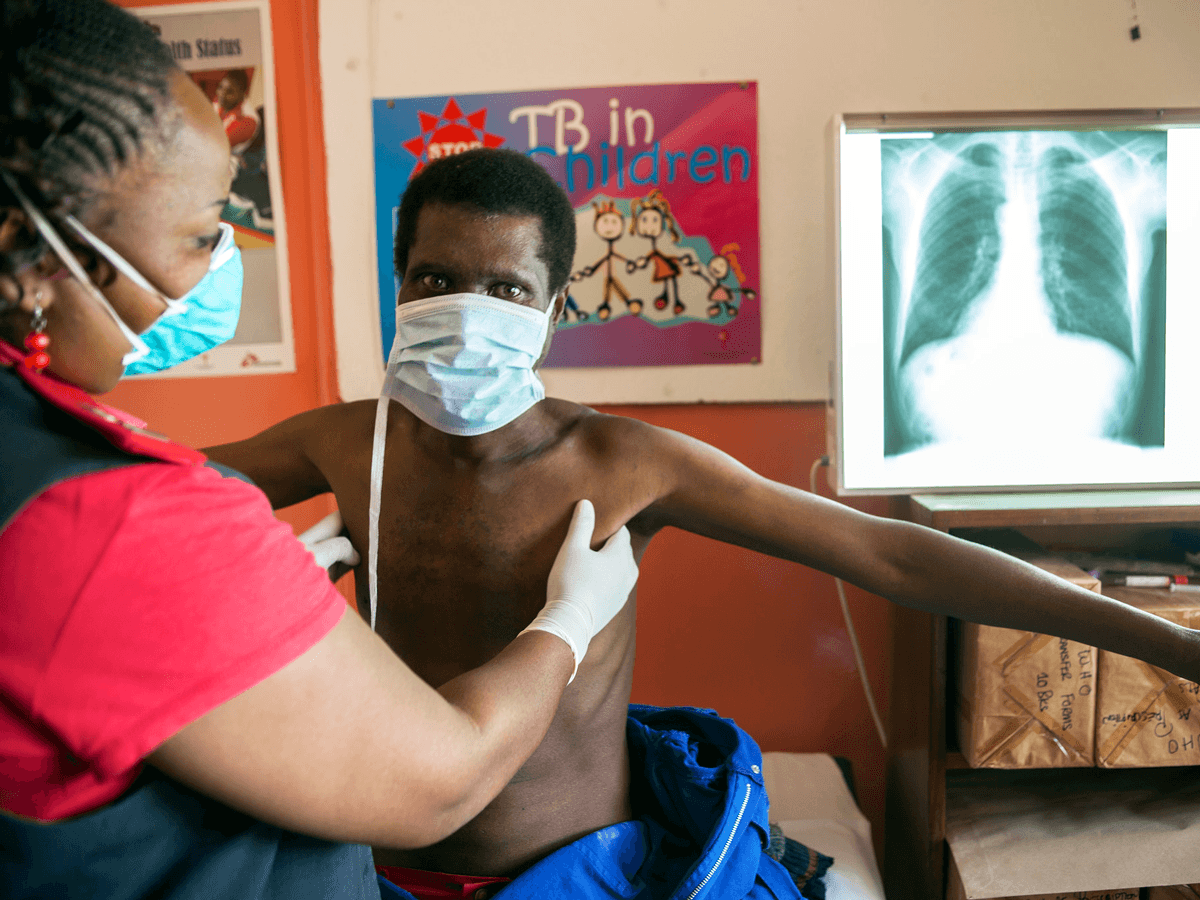
This randomized, double-blind, placebo-controlled trial assessed whether prophylactic prednisone at the time of antiretroviral therapy (ART) initiation could safely reduce the incidence of paradoxical tuberculosis (TB)-associated immune reconstitution inflammatory syndrome (IRIS) among participants with advanced HIV disease receiving TB treatment in South Africa.
Study Setting
- A single government-run outpatient primary care clinic in Khayelitsha, Cape Town, South Africa.
Methods
- Individuals were eligible for enrollment if they were 18 years or older, HIV-positive with a CD4 count ≤100 cells/microliter, initiating ART for the first time, had microbiologically confirmed TB or a clinical diagnosis of TB with a symptomatic response to TB treatment, and had been receiving TB treatment for <30 days.
- Participants were excluded if they were pregnant, had Kaposi’s sarcoma, neurologic or pericardial TB, rifampin-resistant TB, hepatitis B infection, were receiving a nonstandard antituberculosis regimen, had a poor clinical response to TB treatment before the start of ART, had uncontrolled diabetes, had an alanine aminotransferase >200 IU/liter, had an absolute neutrophil count <500/cubic millimeter, or had used systemic glucocorticoids within the previous seven days.
- Participants were randomized (1:1) to receive either 40 mg of oral prednisone daily for 14 days, followed by 20 mg daily for 14 days, started within 48 hours after ART initiation, or placebo.
- The primary end point was the development of paradoxical TB-associated IRIS within 12 weeks after initiating ART, according to the International Network for the Study of HIV-associated IRIS (INSHI) case definition, as adjudicated by a committee of clinical experts.
- Secondary efficacy end points included time to development of TB-associated IRIS, treatment with open-label glucocorticoids for TB-associated IRIS, death from any cause, and hospitalization for any cause.
- Secondary safety end points were severe infections, adverse events, and adverse drug reactions 12 weeks after ART initiation, and HIV-related cancers after one year of follow-up.
- Analyses of the primary end point and secondary efficacy end points used the intention-to-treat approach; safety analyses used the per-protocol approach.
Study Population and Follow-up
- From August 2013 to February 2016, 321 participants were screened, of which 240 were eligible and randomly assigned to receive prednisone (n = 120) or placebo (n = 120).
- The most frequent reasons for exclusion were hepatitis B infection (n = 23) and previous ART (n = 16).
- Fourteen participants in the prednisone group and 13 in the placebo group did not complete the 12-week visit.
- Information on HIV-related cancers after one year was obtained for 220 participants.
- Participants had a median age of 36 (interquartile range [IQR] 30–42), 60% were men, and 73% had microbiologically confirmed TB.
- The median CD4 count was 49 cells/microliter (IQR 24–86), and the median viral load was 5.5 log10 copies/milliliter (IQR 5.2–5.9).
- Participants had received TB treatment for a median of 17 days before starting ART and 97% of participants were treated with tenofovir, emtricitabine (or lamivudine), and efavirenz.
Primary End Point
- In the prednisone group 32.5% (39/120) of participants were diagnosed with paradoxical TB-associated IRIS, compared to 46.7% (56/120) in the placebo group (relative risk [RR] 0.70; 95% confidence interval [CI] 0.51–0.96).
Secondary End Points
- The cumulative incidence of TB-associated IRIS over 84 days was lower in the prednisone group than in the placebo group (hazard ratio 0.61; 95% CI, 0.41–0.92).
- Fewer participants in the prednisone group than in the placebo group were treated for TB-associated IRIS with open-label glucocorticoids (13.3% vs. 28.3%; RR 0.47; 95% CI, 0.27–0.81).
- After 12 weeks, there were five deaths in the prednisone group and four deaths in the placebo group (p = 1.00).
- Fewer participants in the prednisone group than in the placebo group were hospitalized for any cause, but the difference was not significant (14.2% vs. 22.5%; RR 0.63; 95% CI 0.36–1.09).
- A total of 33 severe infections were diagnosed in 29 participants, with 9.2% occurring in the prednisone group and 15.1% in the placebo group (RR 0.61; 95% CI 0.30–1.24).
- There was no significant difference between the groups in adverse drug reactions (RR 1.05, 95% CI 0.61–1.80) or in pre-specified adverse events related to glucocorticoid treatment, with 18 events in the prednisone group and 23 in the placebo group.
- Only one case of Kaposi’s sarcoma was diagnosed after one year, in a participant who was in the placebo group.
Critical Analysis
This randomized, double-blind, placebo-controlled trial demonstrated that four weeks of prophylactic low-dose prednisone started at the time of ART initiation in adults with advanced HIV disease receiving TB treatment reduced the incidence of paradoxical TB-associated IRIS by 30%. An excess risk of severe infections, cancers, or adverse events was not observed, suggesting that this intervention is safe in this population.
The following points should be considered when interpreting the study findings:
- No difference in mortality or hospitalizations was observed between the groups, however the study was not powered to detect differences in these outcomes.
- A quarter of the TB cases were clinically diagnosed, therefore there may have been other underlying opportunistic infections contributing to participants’ initial symptoms and clinical course.
- Despite having advanced HIV disease, study participants were outpatients with good functional status (median Karnofsky performance score 90, IQR 80–90). This may limit the generalizability of these findings to inpatients or more functionally impaired outpatient populations.
- In this trial there were several clinical exclusion criteria, requiring multiple laboratory investigations prior to providing prednisone. This likely contributed to the observed safety outcomes, and may limit the generalizability of these findings to settings in which such tests are not readily available prior to ART initiation.
- In this study, participants were initiating ART within 30 days of starting TB treatment. It is therefore unclear if similar benefits would be seen with prednisone if ART is initiated after 30 days of TB treatment.
Implications
This randomized, double-blind, placebo-controlled trial in South Africa showed that provision of prophylactic prednisone at the time of ART initiation in outpatients with advanced HIV disease receiving TB treatment reduces the incidence of paradoxical TB-associated IRIS. Providers caring for people with advanced HIV disease and TB often have to weigh the benefits of early ART initiation against the risk of IRIS. The relatively simple regimen used in this study could help to mitigate these concerns and significantly reduce IRIS-related morbidity in this high-risk population.
This article synopsis was written by Cassia Wells. Share your thoughts on this article or suggest an article for Journal Club by emailing her at caw2208@columbia.edu
Articles of Note
- Raltegravir-intensified initial antiretroviral therapy in advanced HIV disease in Africa: A randomised controlled trial
- The impact of approaches in improving male partner involvement in the prevention of mother-to-child transmission of HIV on the uptake of safe infant feeding practices by HIV positive women in sub-Saharan Africa. A systematic review and meta-analysis
- Reflexive laboratory-based cryptococcal antigen screening and preemptive fluconazole therapy for cryptococcal antigenemia in HIV-infected individuals with CD4 <100 cells/µL: a stepped-wedge, cluster-randomized trial
- Evaluation of the HIV Infant Tracking System (HITSystem) to optimise quality and efficiency of early infant diagnosis: a cluster-randomised trial in Kenya