Article:
Safety, uptake, and use of a dapivirine vaginal ring for HIV-1 prevention in African women (HOPE): an open-label, extension study
Published in:
Lancet HIV. 2021;8(2):e87-e95
https://doi.org/10.1016/S2352-3018(20)30304-0
Authors:
Baeten JM, Palanee-Phillips T, Mgodi NM, et al for the MTN-025/HOPE Study Team
Summary:
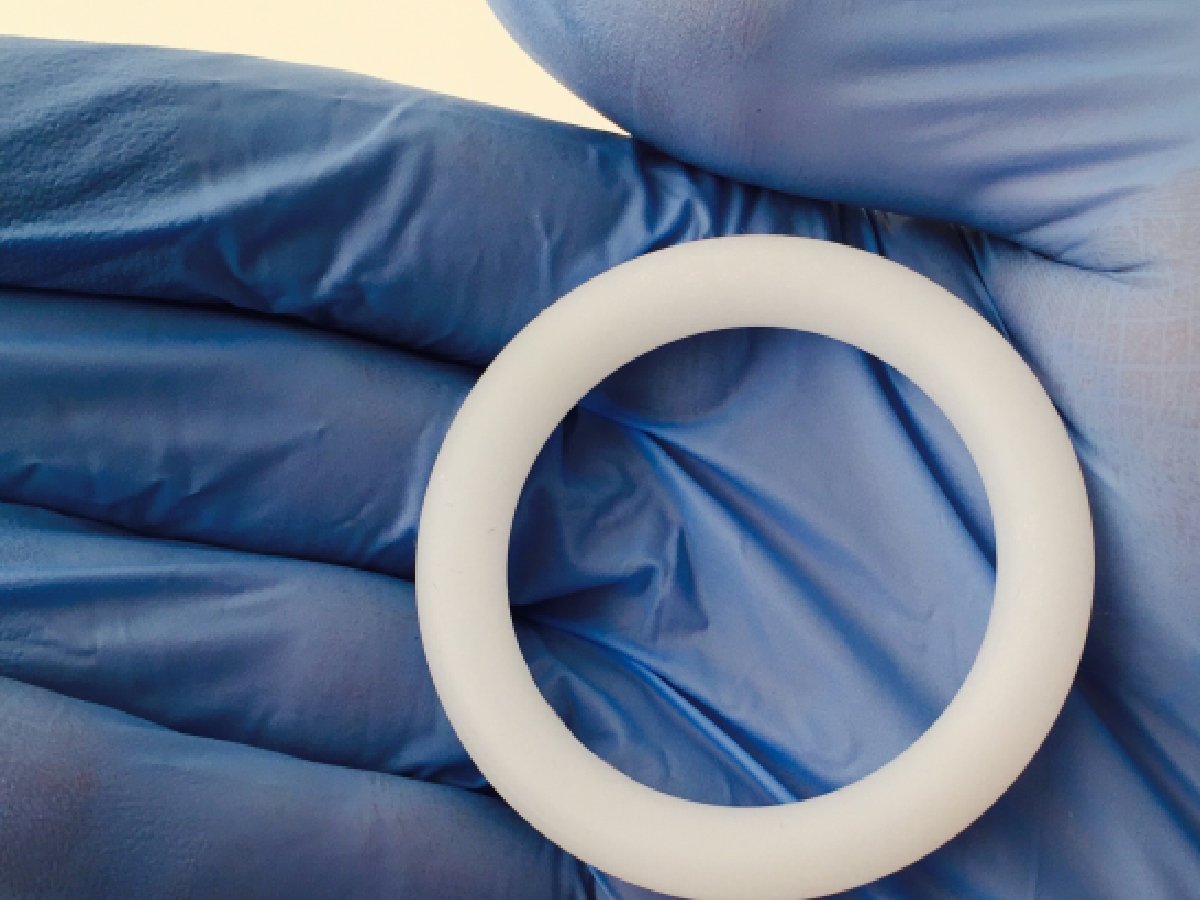
The MTN-025/HIV Open-label Prevention Extension (HOPE) study was a phase 3B, open-label extension trial that evaluated the use and safety of the dapivirine vaginal ring (DVR) in adult women in four African countries. HOPE was conducted following the phase 3, placebo-controlled MTN-020/ASPIRE trial that evaluated the efficacy of the DVR for preventing HIV infection. Eligible women who had completed the ASPIRE study, remained HIV-negative and were not pregnant or breastfeeding were recruited into the HOPE study. Participants were offered access to the DVR for 12 months, and those who accepted were instructed to change the ring monthly and counseled to keep the ring inserted for the entire month. Adherence was measured by the residual amount of dapivirine in returned rings and prevention effectiveness was estimated by comparing the observed rate of incident HIV infections to the expected rate in a similar population without the DVR. The study found high acceptance of the DVR, with greater adherence than was seen in the ASPIRE study and no safety concerns. It was estimated that the DVR reduced incident HIV infections in the study population by 39%. These results, taken together with findings from similar recent studies, suggest that the DVR should be considered as an additional prevention option for women in Africa.
Discussion Questions:
- How could the findings in this study impact policy where you work?
- What would it take to implement this intervention in programs you work with? Do you have any experiences to share?
Please share your thoughts and experiences with us in the comments section below.
Full Synopsis:
PDF version available in English, French, and Portuguese.
Article
Baeten JM, Palanee-Phillips T, Mgodi NM, et al for the MTN-025/HOPE Study Team. Safety, uptake, and use of a dapivirine vaginal ring for HIV-1 prevention in African women (HOPE): an open-label, extension study. Lancet HIV. 2021;8(2):e87-e95. https://doi.org/10.1016/S2352-3018(20)30304-0
Study Summary
The MTN-025/HIV Open-label Prevention Extension (HOPE) study was a phase 3B, open-label extension trial that evaluated the use and safety of the dapivirine vaginal ring (DVR), following the phase 3, placebo-controlled MTN-020/ASPIRE trial that evaluated the efficacy of the DVR for preventing HIV infection in adult women.
Study Setting
- Fourteen clinical research centers in Malawi, South Africa, Uganda, and Zimbabwe.
Methods
- Women who had previously participated in the ASPIRE trial, and remained HIV-negative at the conclusion of the study, were offered screening to participate in HOPE.
- Adult women were eligible to participate in HOPE if they were HIV-negative, using an effective method of contraception, not pregnant or breastfeeding, and otherwise healthy, with no contraindications to use of the DVR, including no safety concern requiring permanent product discontinuation while participating in ASPIRE.
- Those who enrolled in HOPE were offered 12 months of access to the 25mg DVR.
- Study visits occurred at enrollment, followed by monthly for three months, and then once every three months. At each visit, women were counseled that they could choose to accept or decline the DVR at any point and still continue in the study.
- Participants choosing to accept were provided with a sufficient number of DVRs to last until their next scheduled visit, were taught how to insert and remove the vaginal ring, were instructed to change the ring monthly and counseled to keep the ring inserted for the entire month.
- Counseling about the DVR as an HIV prevention option was provided in combination with comprehensive counseling on HIV prevention, including behavioral change for risk reduction, partner HIV testing, testing and treatment of sexually transmitted infections (STIs) in participants and partners, and the offer of free condoms. Referrals were also provided to access oral pre-exposure prophylaxis (PrEP) through local clinics at enrollment or at any time during follow-up.
- Participants were instructed to return used rings at scheduled follow-up visits, which also included HIV serological testing, safety monitoring, pregnancy testing and individualized adherence counseling. The DVR was withheld from women if there was a clinical safety concern, or if they became pregnant until they were no longer pregnant or breastfeeding.
- Participants completed a final study visit four weeks after the last study product use visit to assess for delayed HIV seroconversion. Archived plasma samples from visits before seroconversion were tested, including resistance testing, and participants with detectable HIV-1 RNA at enrollment were excluded as primary study endpoints.
- The primary adherence endpoint was amount of dapivirine released from returned rings, calculated by residual dapivirine present, and categorized as ≤0.9 mg (no use), >0.9 mg to 4.0 mg (some use), and >4.0 mg (28 days of continuous use).
- Adherence data were assessed over time, including assessment of consistent use (defined as ≥0.9 mg dapivirine released from all three rings in three months) and persistent use (defined as ≥0.9 mg dapivirine released from all three rings in three months for all 12 months of follow-up).
- Safety was evaluated in the subset of participants who ever received a DVR during the study and the primary safety endpoint was a composite of any serious adverse event, any grade 3 and 4 adverse events, and grade 2 adverse events assessed by the study clinicians as related to the study product.
- Additional outcomes included uptake and acceptance of the DVR at enrollment and during follow-up, as well as incident HIV acquisition, which was compared to an expected counterfactual HIV incidence in a simulated population with similar risk.
Study Population and Follow-up
- Women were enrolled between July 2016 and October 2018. Of the 2,448 potentially eligible ASPIRE participants, 2,263 (92.4%) were approached for participation in HOPE, of which 507 (22.4%) were not screened.
- Common reasons for not being screened included pregnancy, intending to become pregnant, or breastfeeding (n=189); declined screening (n=134); relocation or work commitments that prevented participation (n=122) and self-reported HIV acquisition since ASPIRE (n=27).
- In total, 1,756 were screened, of whom 183 (10.4%) were ineligible (69 pregnant or breastfeeding, 45 HIV-positive, 69 other reasons), 117 (6.7%) declined study participation, and 1,456 (82.9%) were enrolled.
- Of enrolled women, 48.6% were from South Africa, 28.8% were from Zimbabwe, 11.8% were from Uganda and 10.8% were from Malawi, which was similar to the distribution in ASPIRE.
- The median age of participants was 31 years (interquartile range [IQR] 27–37), 47.1% were married, 43.3% reported condom use with the last sex act, and 15.8% had a curable STI at study screening.
- Oral PrEP use was reported by 16 women at 36 visits during HOPE.
- Participants completed 8,436 (97.9%) of 8,621 expected follow-up visits.
Acceptance Outcomes
- At enrollment, 92.2% of women accepted the DVR and acceptance of the ring remained high throughout follow-up: 90.1% at month 1, 88.5% at month 2, 86.9% at month 3, 83.3% at month 6, and 79.3% at month 9.
- Excluding women who acquired HIV or who had another medical reason for not using the ring, 73.2% of women accepted the ring for all 12 months of follow-up.
- At visits where the ring was not accepted, the most common reasons given by participants were: preference for alternative HIV prevention strategies (42.6% of visits); not interested in receiving the ring (20.4% of visits); not ready to receive the ring (13.7% of visits); partner unsupportive of ring use (10.9% of visits); and other reasons (14.3% of visits).
- Rarely reported reasons for declining the DVR were: side-effects (3.7% of visits); feeling the ring was less effective than desired (2.2% of visits); intending to fall pregnant (0.7% of visits); and an unsupportive family (0.2% of visits).
Adherence Outcomes
- Of 14,463 rings dispensed, 99.7% were returned and 97.0% were tested for residual amounts of dapivirine.
- Overall, 89.3% of rings tested had >0.9 mg of dapivirine released, indicating at least some use.
- The median amount of dapivirine released was 3.2 mg (IQR 2.4-4.3) and was relatively unchanged throughout the 12-month follow-up period.
- Returned rings from HOPE had a mean of 0.21 mg more dapivirine released than ASPIRE (95% confidence interval [CI] 0.18–0.25; p<0·0001).
- Consistent and persistent use was evaluated in 1,277 participants, with 4,595 evaluations of three-month use completed. Of these evaluations, 77.0% had evidence of use throughout the 3 months (77.0% in months 1-3, 79.9% in months 4-6, 78.3% in months 7-9, and 72.1% in months 10-12).
- Overall, 44.0% of the 1,277 women were classified as having persistent use through all 12 months of follow-up.
- Age and self-reported behavioral risk factors for HIV were not associated with poorer use, whereas consistent use in the previous 3 months strongly predicted subsequent consistent use.
- Adjusted for site and age, women who accepted the ring at all study visits had a mean of 0.72 mg (95% CI 0.57-0.88; p<0.0001) more dapivirine released from rings than women who inconsistently accepted.
Safety Outcomes
- Serious adverse events occurred in 19 (1.4%) participants, over 22 events, and no serious adverse event or ≥grade 3 adverse event was assessed to be related to the use of the DVR.
- Grade 2 adverse events assessed as related to the DVR occurred in two participants, with abdominal pain (n=1) and pelvic pain with DVR insertion (n=1).
- The primary composite safety endpoint events occurred in 54 (3.9%) participants, and the frequency, severity, and type of adverse events observed were similar to those seen in the ASPIRE trial, with no new safety signals observed.
Incident HIV Outcomes
- There were 35 incident HIV infections in the study population, at an incidence of 2.7 per 100 person-years (95% CI 1.9-3.8).
- Counterfactual simulations based on data from the placebo group of ASPIRE predicted a median incidence of 4.4 per 100 person-years (95% CI 3.2-5.8) and thus the reduction in HIV incidence in HOPE was estimated to be 39% (95% CI 14–65).
- Among the 35 infections, seven had non-nucleoside reverse transcriptase mutations, none of which suggested a dapivirine-specific resistance pattern.
Critical Analysis
The multicenter, open-label extension HOPE trial evaluated use and safety of the DVR for HIV prevention, in women who had previously participated in the phase 3 ASPIRE trial. Findings suggest high uptake of the DVR in this population, greater adherence compared to ASPIRE and evidence of persistent use throughout the 12 month study period. The DVR was also well-tolerated and had a safety profile consistent with that seen in ASPIRE. Although HOPE was not a placebo-controlled trial, a lower number of incident HIV infections than would be expected in the absence of the ring was observed.
The following points should be considered when interpreting the study findings:
- Phase 3 trials showed that the DVR reduced HIV incidence by approximately 30% compared with placebo, and by 50% or more among subgroups with evidence of greater adherence to ring use.1, 2 By contrast, HOPE estimated a reduction in HIV incidence of 39% across the entire study population, including those not accepting or not using the DVR. Although limited by the lack of a placebo group, this estimate suggests slightly higher effectiveness when the DVR is used in an open-label setting, similar to findings from the open-label DREAM study.3
- While acceptance rates of the DVR were high in this population, all these women had experience with vaginal rings, having successfully completed the ASPIRE trial, limiting the generalizability of these findings.
- Similarly, while adverse events were rare, women who had previous safety concerns related to the ring in ASPIRE were excluded from HOPE, which may limit generalizability of the safety data from this study.
- ASPIRE concluded follow-up in June 2015 and HOPE initiated enrollment in August 2016, concluding enrollment in May 2018. The study population consisted of women who remained HIV-negative throughout ASPIRE, and in the interim period between ASPIRE and HOPE. This approach to recruiting could have selected for a population with below-average risk of acquiring HIV, which may limit generalizability of the effectiveness findings.
- In ASPIRE, objective measures of adherence and HIV risk reduction were lowest among women aged 18–21 years. The HOPE recruitment strategy meant that very few women were still in this age group at enrollment, limiting the study’s ability to assess outcomes in younger women.
- Pregnant and breastfeeding women were excluded from this trial, therefore the safety, acceptability and effectiveness of the DVR in this population remains unknown.
- While DVR acceptance was high and adherence was greater in HOPE compared with ASPIRE, less than half of the women in HOPE were classified as having persistent use of the DVR during all 12 months of follow-up. This suggests that providing women with a menu of HIV prevention options will remain important if the DVR becomes widely available.
- The use of oral PrEP was permitted in this study, however it was generally not available in public sector settings and very few women were taking oral PrEP. It therefore remains to be seen what impact oral PrEP availability would have on the uptake of the DVR in this population.
Implications
The multicenter, open-label extension HOPE trial evaluated the use and safety of the DVR for HIV-negative women in four African countries and found high levels of acceptance and greater adherence compared to the phase 3, placebo controlled ASPIRE trial. There was also evidence of improved effectiveness at preventing HIV when the DVR was used in an open-label setting. These results, combined with similar results from the recent DREAM study,3 suggest that regulatory bodies should consider the DVR as an HIV prevention option for women living in similar settings. Although the DVR is less efficacious at preventing HIV infection than daily oral PrEP, an additional, women-centered prevention option would be valuable to meet the needs of those unable or unwilling to take daily PrEP.
References
1) Baeten JM, Brown ER, Hillier SL. Dapivirine vaginal ring for HIV-1 prevention. N Engl J Med. 2017; 376: 995–96.
2) Nel A, van Niekerk N, Kapiga S, et al. Safety and efficacy of a dapivirine vaginal ring for HIV prevention in women. N Engl J Med. 2016; 375: 2133–43.
3) Nel A, van Niekerk N, Van Baelen B, et al. Safety, adherence, and HIV-1 seroconversion among women using the dapivirine vaginal ring (DREAM): An open-label, extension study. Lancet HIV. 2021;8(2):e77-e86.
This article synopsis was written by Cassia Wells. Share your thoughts on this article or suggest an article for Journal Club by emailing her at caw2208@cumc.columbia.edu
Articles of Note:
- HIV clinic-based buprenorphine plus naloxone versus referral for methadone maintenance therapy for treatment of opioid use disorder in HIV clinics in Vietnam (BRAVO): an open-label, randomised, non-inferiority trial
- Safety, adherence, and HIV-1 seroconversion among women using the dapivirine vaginal ring (DREAM): an open-label, extension study
- Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia
- Randomized Trial of a Vaccine Regimen to Prevent Chronic HCV Infection
- Repurposed Antiviral Drugs for Covid-19 — Interim WHO Solidarity Trial Results