Article and Study Summary
Community based distribution of oral HIV self-testing kits in Zambia: a cluster-randomised trial nested in four HPTN 071 (PopART) intervention communities.
Published in:
Lancet HIV. 2019;6(2):e81–e92.
DOI: 10.1016/S2352-3018(18)30258-3
Authors:
Mulubwa C, Hensen B, Phiri MM, et al., for the HPTN 071 (PopART) Study Team
Summary:
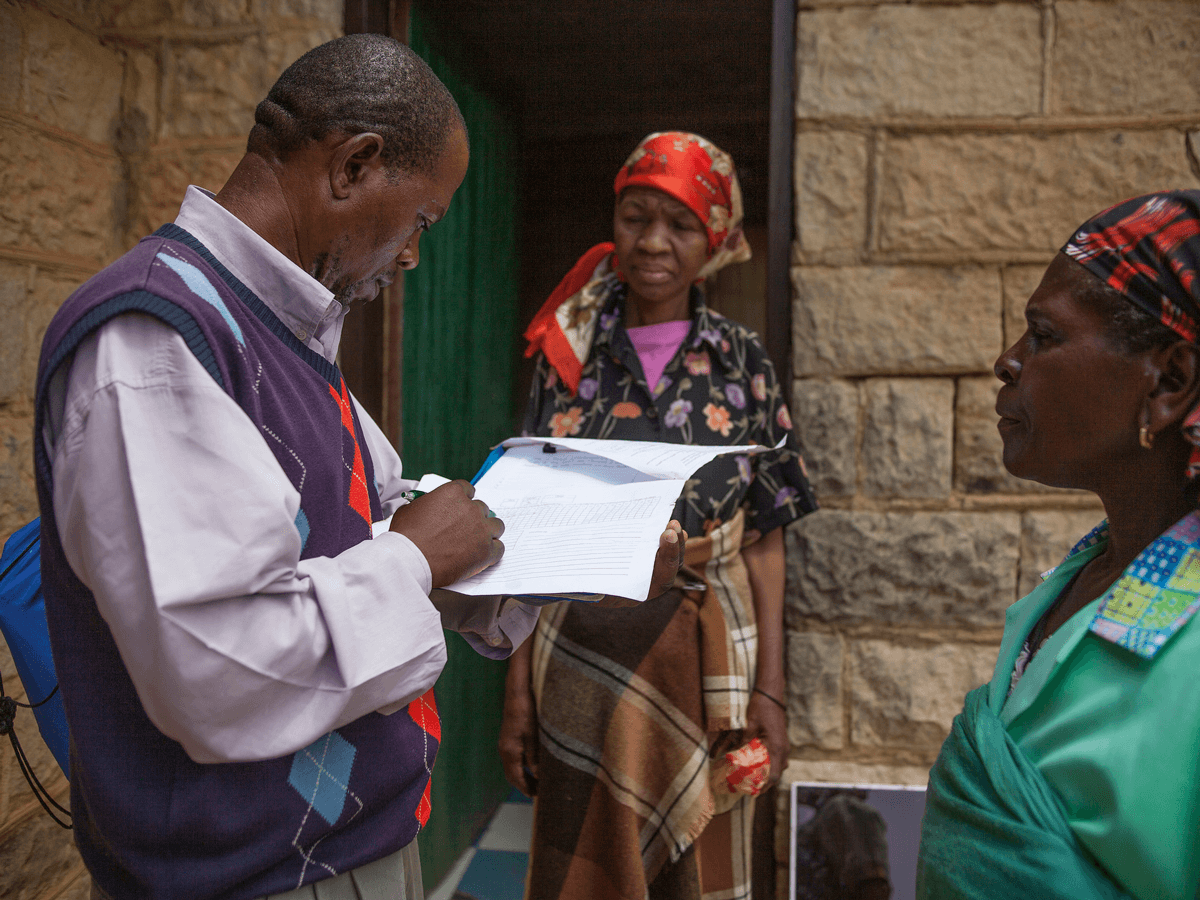
This article reports on a cluster-randomized trial, nested within the HPTN 071 (PopART) study, that evaluated the effect of offering door-to-door HIV self-testing (HIVST) on knowledge of HIV status among four communities in Zambia. Over a three-month period, communities were randomized to either receive the standard PopART intervention, which included community HIV care providers offering door-to-door home-based HIV testing services, or the standard PopART intervention plus the option of HIVST as an alternative mode of testing. Household members opting for self-testing could choose supervised or unsupervised use of the HIVST kit, and those with partners not present during the visit could keep a kit for secondary distribution to partners. The primary outcome of interest was knowledge of HIV status among household members aged 16 years or older. The results showed a small but significant increase in knowledge of HIV status in the HIVST group. This effect was driven by more men knowing their HIV status in the HIVST group, many of whom were not present at the time of the initial home visit. Men aged 30 years or older were more likely to self-test through unsupervised use or from secondary distribution of HIVST kits compared to younger age groups. These results suggest that community-based door-to-door distribution of HIVST kits can play a role in accessing men who may otherwise be difficult to reach with regular HIV testing services.
Discussion Questions:
- How could the results presented in this article inform the programs that you work with?
- What programmatic challenges do you foresee in implementing a similar intervention as the one described in this study? Do you have any experiences to share?
Please share your thoughts and experiences with us in the comments section below.
Full Synopsis:
PDF version available in English, French, and Portuguese.
Study Summary
This nested cluster-randomized trial evaluated whether offering HIV self-testing (HIVST) at the time of offering door-to-door HIV testing services (HTS) in the home increased knowledge of HIV status among household members, compared to offering home-based HTS alone.
Study Setting
- Four urban communities in two northern provinces of Zambia that were in the intervention arm of the HPTN 071 (PopART) trial.
- PopART is a cluster-randomized trial in 21 communities in South Africa and Zambia aiming to estimate the effect on HIV incidence of a household-based combination HIV prevention package, which includes offering annual door-to-door home-based HTS, linkage to immediate treatment for HIV-positive individuals, and promotion of male circumcision for HIV-negative men.
- The four communities were divided into 66 zones (clusters) that included approximately 450-500 households each, with an estimated total population of 90,000 individuals aged 16 years or older.
- Communities had previously undergone two rounds of the PopART intervention and were selected to be representative of the range and pattern of HTS uptake in other PopART intervention communities.
Methods
- All residents of the 66 zones aged 16 years or older were eligible to participate in the HIVST study, which was nested within the third round of the PopART trial over a three-month period.
- The 66 zones were randomized (1:1) to either the HIVST group or the non-HIVST group. Randomization was stratified within and across communities to achieve balance based on key outcomes documented in round 2 of the PopART trial.
- The non-HIVST group received the PopART intervention. Community HIV care providers went door-to-door to each household, where they enumerated household members and provided an intervention package, which included offering HTS with a finger-prick rapid diagnostic test (RDT) to eligible residents. Providers returned to households to offer HTS to residents who were not present during the first visit.
- The HIVST group received the routine PopART intervention package, but were offered a choice of using oral HIVST instead of routine HTS via finger-prick RDT.
- Household members who opted for HIVST could choose supervised or unsupervised use of the HIVST kit.
- Individuals aged 18 years or older were offered an additional HIVST kit for secondary distribution to their partner, if the partner was absent at the time of the visit and resided in the same household.
- Those opting for HIVST were given a demonstration by the community HIV care provider, an HIVST kit with pictorial instructions, a card with the community HIV care provider’s phone number, a results form to complete, and an envelope for returning the used HIVST.
- Those accepting an HIVST kit for their partner were asked to sign an agreement stating that it would only be given to the intended individual, that the individual would not be coerced into using it, and that the information required for the individual to use the HIVST kit would be conveyed. The community HIV care provider also left a card with their phone number for the absent individual to contact them if additional support or confirmatory testing was required.
- For those choosing unsupervised HIVST, or who were given a test for secondary distribution, the community HIV care provider conducted a follow-up visit seven days later to ascertain if the kit was used, collect result forms if available, and offer confirmatory testing for any reactive HIVST results. The community HIV care provider also attempted to meet with partners who received the kits via secondary distribution, if possible.
- Those who were left an HIVST kit were followed up for five months after the end of the intervention period.
- The primary outcome of interest was knowledge of HIV status among enumerated household members, defined as self-reported HIV positive status or accepting either HIVST or finger-prick RDT, with results documented.
- Secondary outcomes included uptake of HTS among eligible individuals, linkage to confirmatory testing in the HIVST group, incremental cost of adding HIVST to the PopART intervention, and social harms.
Study Population and Update of HIVST
- Between February and April 2017, the community HIV care providers enumerated 13,267 eligible individuals in the HIVST group and 13,706 in the non-HIVST group.
- In both groups, half the individuals were aged 16–29 years and half were men.
- A similar proportion of household members were absent during the community HIV care provider’s visit in both groups (21% in the HIVST group and 22% in the non-HIVST group), of which the majority were men (70% and 71%, respectively).
- Of the 9,020 individuals in the HIVST group who were seen and eligible for HIV testing, 4,238 (47%) opted for HIVST, of which 3,737 (88%) were supervised tests.
- An additional 323 household members (283 males, 40 females) received an HIVST kit through secondary distribution and had documented results; for 242 (75%) results were obtained via their partner, and for 81 (25%) results were obtained in person.
Primary Outcome
- After the intervention period, 68% of individuals in the HIVST group knew their HIV status compared with 65% in the non-HIVST group (adjusted odds ratio [aOR] 1.30, 95% confidence interval [CI] 1.03–1.65).
- Among men, knowledge of HIV status was higher in the HIVST group than in the non-HIVST group (60% vs. 55%, aOR 1.31, 95% CI 1.07-1.60), whereas among women there was no difference between groups (75% vs. 75%, aOR 1.05, 95% CI 0.86–1.30; p = 0.01 for interaction).
- The effect did not differ by age group (p = 0.44 for interaction); however, more adults aged 16–29 years (74%) and aged 30 years or older (62%) knew their HIV status in the HIVST group, compared to the non-HIVST group (70% and 60%, respectively).
- Among individuals who were resident during PopART rounds 1 and 2, but did not participate in either round, a greater number in the HIVST group had knowledge of their HIV status compared with the non-HIVST group (30% vs. 21%, aOR 1.63, 95% CI 1.15–2.31).
Secondary Outcomes
- Offer of HIVST increased acceptance of HTS among eligible men (aOR 1.42, 95% CI 1.10–1.85), but not women (aOR 1.05, 95% CI 0.82–1.35), and the effect was similar across age groups in men.
- Among men who self-tested, 38% of those aged 30 years or older used unsupervised or secondary distribution of HIVST kits, compared with 17% of men aged 16–29 years (p = 0.004).
- Among the 148 individuals whose first HIVST result was reactive, 5% subsequently reported they knew they were HIV positive, and 2% repeated HIVST after meeting the community HIV care providers and the test result was negative. Of the remaining 138 who were eligible for confirmatory HIV testing, 76% linked to confirmatory testing, of whom 97% were confirmed HIV positive.
- The incremental cost of distributing HIVST kits door-to-door, alongside routine door-to-door HTS, was estimated to be $255.98 per additional person tested, amounting to $771.88 per person confirmed HIV positive.
- Thirteen social harms were reported in the HIVST group, including invasion of privacy, emotional distress, being deceived or forced into doing HIV testing, threatened or actual violence, and separation of couples.
Critical Analysis
This cluster-randomized trial demonstrated that offering a choice of HIVST while delivering home-based HTS resulted in a small but significant increase in knowledge of HIV status among the general population aged 16 years or older. This increase was driven by an effect in men, many of whom were not present during a home visit and benefitted from secondary distribution of HIVST kits via their partners.
The following points should be considered when interpreting the study findings:
- This effect was observed despite these communities having previously undergone two rounds of the PopART intervention, which provided convenient door-to-door home-based HTS. Offering home-based HIVST may have a greater effect on knowledge of HIV status in communities with less convenient HIV testing alternatives.
- Community saturation with HIV testing in the previous two years likely reduced the yield and contributed to the higher incremental cost per positive identified.
- HIVST distribution included an in-person demonstration and close in-person follow-up by community HIV care providers, which is resource-intensive and may limit generalizability to other HIVST distribution models.
- While this study provides promising evidence for secondary distribution of HIVST kits, this option was limited to those living with their partners, and extra steps were taken to avoid diversion of kits or coercion. This may limit generalizability of these findings in other contexts offering secondary distribution of HIVST kits.
- Despite resource-intensive follow-up procedures, a quarter of those with reactive HIVST results did not get confirmatory testing.
- The community HIV care providers had established long-term relationships with these households, likely contributing to trust with household members. This likely increased the acceptability of HIVST among residents, and may limit generalizability of these findings in other contexts.
Implications
This cluster-randomized trial, nested within the PopART study, found that community-based, door-to-door distribution of HIVST kits increased knowledge of HIV status among men in a population that was already receiving home-based testing services. Men who are not home when services were offered benefited the most, suggesting that HIVST is a promising way to reach men who cannot be reached for services during regular hours. This study also found that uptake of unsupervised HIVST was higher among men aged 30 years or older, suggesting that this method may be a way to reach this age group. However, despite intensive follow-up, challenges remained with confirmatory retesting. Programs should consider community-based distribution of HIVST kits to engage hard-to-reach men, but also need to strengthen measures to ensure follow-up of test results and linkage to care.
This article synopsis was written by Cassia Wells. Share your thoughts on this article or suggest an article for Journal Club by emailing her at caw2208@columbia.edu
Articles of Note
- Financial incentives for achieving and maintaining viral suppression among HIV-positive adults in Uganda: a randomised controlled trial
- Impact of routine cryptococcal antigen screening and targeted preemptive fluconazole therapy in antiretroviral-naive human immunodeficiency virus–infected adults with CD4 cell counts <100/μL: a systematic review and meta-analysis
- HIV self-testing alone or with additional interventions, including financial incentives, and linkage to care or prevention among male partners of antenatal care clinic attendees in Malawi: An adaptive multi-arm, multi-stage cluster randomised trial
- Discontinuing cotrimoxazole preventive therapy in HIV-infected adults who are stable on antiretroviral treatment in Uganda (COSTOP): A randomised placebo controlled trial