Across the world, the introduction of antiretroviral therapy (ART) and the progress made to HIV service delivery transformed a once-deadly disease into a chronic, manageable condition—presenting a hopeful future where people living with HIV could live long, healthy, and productive lives.
Despite this remarkable progress, curbing new infections has remained a persistent challenge. Every year, an additional 1.7 million people all over the world acquire HIV. This high incidence rate, particularly among members of key populations, shows that although access to critical, lifesaving medications has improved all over the world, global HIV prevention strategies have lagged sorely behind, calling for new tools and innovations.
Oral Pre-exposure Prophylaxis, or PrEP—most frequently prescribed as daily emtricitabine and tenofovir disoproxil fumarate, is one such innovation with the potential to stem the tide of new HIV infections around the world. PrEP was first approved for use by the U.S. Food and Drug Administration in 2012.
PrEP’s introduction was met with relief, enthusiasm, and curiosity.
“I think PrEP is such a monumental tool because up until this point, so much has been focused around treatment,” said Halli Olsen, MPH, global technical assistance clinical coordinator at ICAP. “On the prevention side, it felt like people were losing a bit of hope. PrEP was the first tool that came out in years that gave people an option.”
ICAP champions the use of PrEP as part of combination HIV prevention through multiple research and programmatic awards, including the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC). To support PrEP implementation, ICAP developed the PrEP Package, a comprehensive toolkit including training materials, job aids, and monitoring and evaluation tools designed to enable clinical providers to provide PrEP to appropriate candidates in a safe and effective manner. The package is adaptable to specific contexts and available in English, Spanish, French, and Portuguese.
PrEP is a powerful addition to a comprehensive biomedical prevention package that includes regular use of condoms, routine HIV testing, and voluntary male circumcision. Though not a ‘standalone’ solution to reducing the risk of HIV, the value of PrEP lies in its effectiveness and the peace of mind it can bring to individuals at risk.
Harnessing Lessons Learned in ART Service Delivery to Inform PrEP Implementation Models

At ICAP’s Harlem Prevention Center, a study was conducted with individuals at risk of HIV infection to assess their experiences with PrEP
ICAP’s decades of HIV prevention, care, and treatment work and innovations in ART delivery and scale-up laid the groundwork for integrating PrEP into a robust continuum of services, including targeted HIV testing, whereby individuals who are at risk and test negative have the option to start PrEP.
ICAP continues to build on lessons-learned in ART delivery to ensure that PrEP services are feasible, responsive to the daily realities of people’s lives, and that clinicians and health workers are trained in identifying appropriate candidates for PrEP.
To build the type of formative research needed to design effective PrEP implementation programs, ICAP has been conducting acceptability and dosing studies. One such study, HPTN 067, supported by the HIV Prevention Trials Network (HPTN) and funded by the National Institutes of Health (NIH), assessed the acceptability of non-daily dosing for PrEP, including a regimen of pill-taking before and after potential exposure to HIV, similar to the dosing strategy recently demonstrated effective and approved for men who have sex with men (MSM), a key population at risk for HIV.
HPTN 067 also provided insight into the structural and social barriers that can impact PrEP adherence, particularly for MSM. The study, also known as the Alternate Dosing to Augment Pre-Exposure Prophylaxis Pill Taking (ADAPT) raised important considerations about sensitization and community engagement—factors that ICAP took into account as it began embarking on global PrEP implementation.
Successes and Challenges in Global PrEP Implementation

A pharmacy in the Democratic Republic of Congo, where outreach services are successful in linking key populations to PrEP services
Despite the many differences in use of antiretrovirals as PrEP and as treatment for HIV infection, there are some shared challenges in the implementation of ART and PrEP. With both, retention and adherence are enduring uphill battles, and, with PrEP, the complexity of these challenges can be amplified given the random, noncontinuous nature of potential HIV exposure.
“It’s very hard to get someone who is negative and healthy to come to the clinic,” said Cassia Wells, MD, MPH, MA, clinical officer at ICAP. “This is true for any preventive medicine. Getting people who feel fine to take a daily medication for preventive purposes is not easy.”
ICAP assisted in PrEP implementation in five countries as part of the Global Technical Assistance (GTA) Project, supported by PEPFAR through CDC. Though similar challenges in loss to follow up existed, the results in some contexts were surprising. In the Democratic Republic of Congo (DRC), where ICAP supported the first PrEP services with funding from PEPFAR through CDC, existing programs were leveraged with support from the DRC Ministry of Health to train health care workers in delivering PrEP to key populations, as well as appropriate monitoring and follow-up with participants. Retention at one- and three-month follow-up visits was then assessed. The results were positive, with a 93 percent retention rate at three-month follow-up (a 15 percent increase from retention at one month).
One key factor in the success: community outreach.
“In DRC, the health care workers didn’t just conduct outreach, they built relationships, going door to door and working directly with people,” said Julie Franks, PhD, senior research associate at ICAP. “The clinics had the type of relationship with key population clients that usually only exists with lifelong ART clients. The staff were highly skilled at developing relationships and were able to leverage those engagement techniques to keep people in care.”
In Mozambique, ICAP assisted the Ministry of Health in the phased implementation of PrEP, adapting training materials to fit the country context. As part of ICAP’s care and treatment project in Mozambique, a pilot in Zambézia province is focused on serodiscordant couples at ART clinics—creating a “one-stop-shop” model at health facilities where individuals in serodiscordant relationships were linked to PrEP and other services.
Because stigma is an ongoing obstacle preventing many key populations who are drivers of the HIV epidemic from seeking both prevention and treatment services, weaving PrEP within community-based service delivery models may be an effective way to reach individuals where they are with medication that could alter their lives.
Targeted community outreach has also proven to yield positive results in ICAP’s Tanzania-based project known as FIKIA (“to reach” in Swahili), where a community-based delivery model was adopted to integrate PrEP into existing ART outreach programs. For female sex workers in rural Tanzania, access to PrEP has become an empowering and anxiety-reducing revelation—allowing them to earn a living while protecting themselves against HIV.
“In PrEP implementation, we are learning from ART differentiated service delivery models—we need to make it easier for people to get PrEP and make sure it fits seamlessly into their lives,” said Wells.
“Regardless of people’s experiences with PrEP, if you get them engaged in one form of prevention, and reduce their anxiety, they will likely be open to other forms of prevention as well,” added Franks. “For me, that’s one of the most important messages I took away from the contraceptive field—once you get people into the flow, they will continue to seek preventive care.”
What’s Next? Innovations in Communication and Delivery
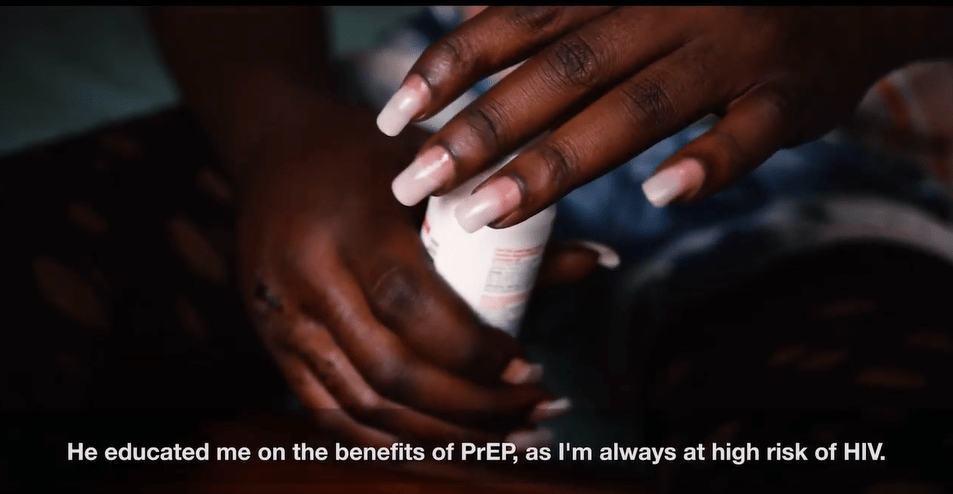
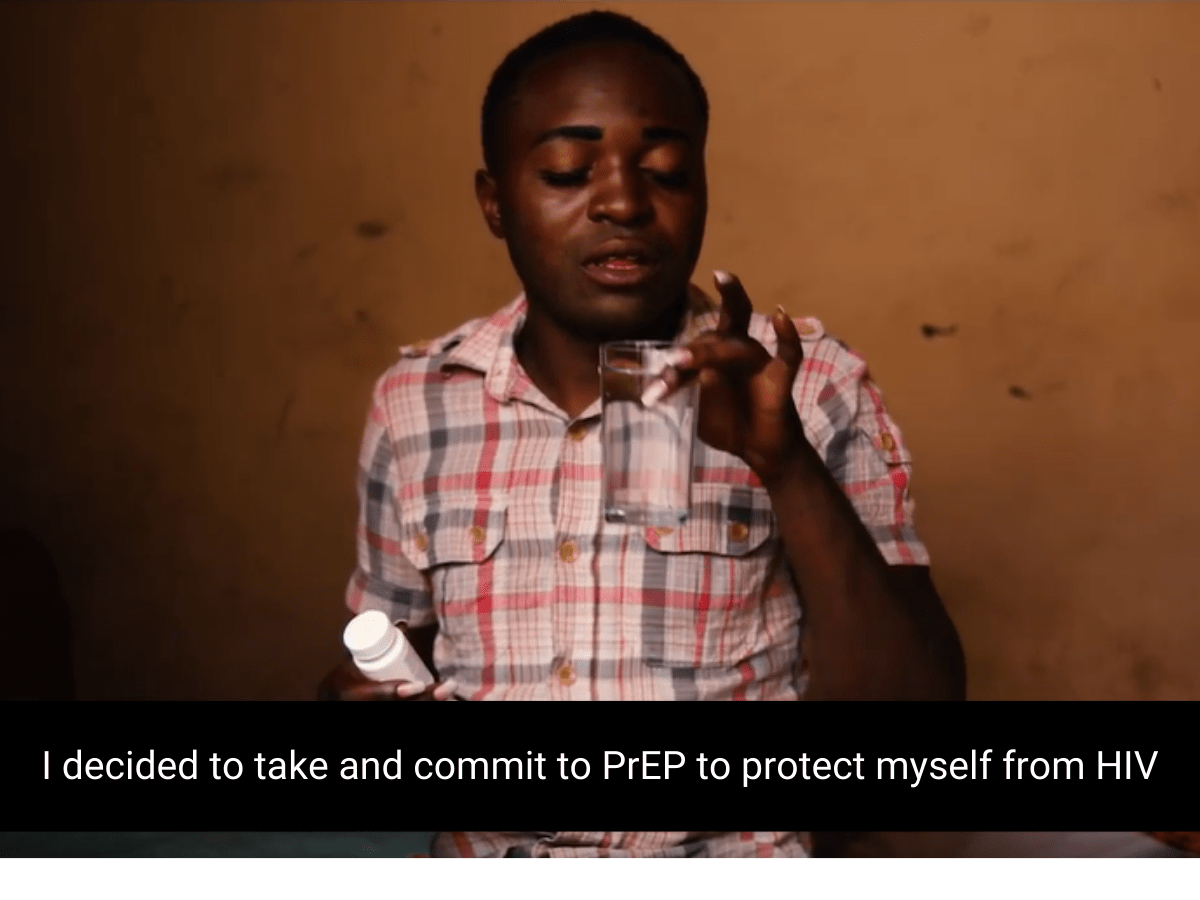
A male sex worker in DRC shares his experiences with taking PrEP in the ‘Power of PrEP’ video series, featuring stories from at-risk individuals in three different countries
Nuanced communication across different platforms and countries is needed in order to reach appropriate candidates with PrEP. Demand-creation videos, such as ICAP’s “Power of PrEP” series, supported by PEPFAR through CDC as part of the GTA project, can be effective tools to destigmatize the use of PrEP and reiterate the idea that PrEP is for anyone who wants to stay healthy in the face of risk.
Additionally, leveraging digital technology is a powerful way to increase adherence and retention. In Tanzania, with an entirely community-based model and no fixed location to deliver PrEP, social technology such as WhatsApp has shown outstanding results in diminishing loss to follow-up.
“Because the culture of texting is so ingrained, sending a message to someone the second or third day after they start PrEP and simply asking ‘how are you doing?’ is such an easy, low-resource way to show you care and are in touch,” said Franks.
In Kisumu, Kenya, a new ICAP study in collaboration with the community-based group, Impact Research and Development Organization, will further investigate the impact of peer-based support through texting on PrEP coverage among a highly-mobile female sex worker population surrounding Lake Victoria.
Innovations in PrEP delivery, such as long-acting injectable PrEP, are also beginning to make rounds, revolutionizing the possibilities for adherence and retention. In Eswatini, ICAP launched a groundbreaking study with HPTN and the Eswatini Ministry of Health, evaluating the safety and efficacy of the long-acting injectable PrEP, evaluating its safety and efficacy among HIV-negative women. A parallel HPTN study of long acting injectable PrEP for MSM and transgender women is being conducted at ICAP research sites in Harlem and the Bronx, New York.
Continually expanding upon and finding new ways to prevent the spread of HIV is crucial to prevent new infections. With this in mind, expanding PrEP beyond key population members, and emphasizing that the drug is for anyone experiencing ongoing, substantial risk to HIV, is critical to reduce stigma and increase uptake.
“There’s a school of thought in PrEP that derives from the experience of introducing new products like oral contraceptives into family planning,” Franks noted. “From that perspective, PrEP is still in the early ‘diffusion’ stage where there are many questions about its effectiveness and appropriate use. We need to keep going until it does become normalized and there is a reversal of stigma, and we need to continue to be thoughtful about how we engage and how we reduce barriers to preventive care.”
Downloadable Resources Featured in this Piece:
ICAP’s four-part Test and Treat All compendium
ICAP’s Key Populations Technical Brief
ICAP’s PrEP Package – version 3.0 now available
ICAP’s PrEP Technical Brief