-
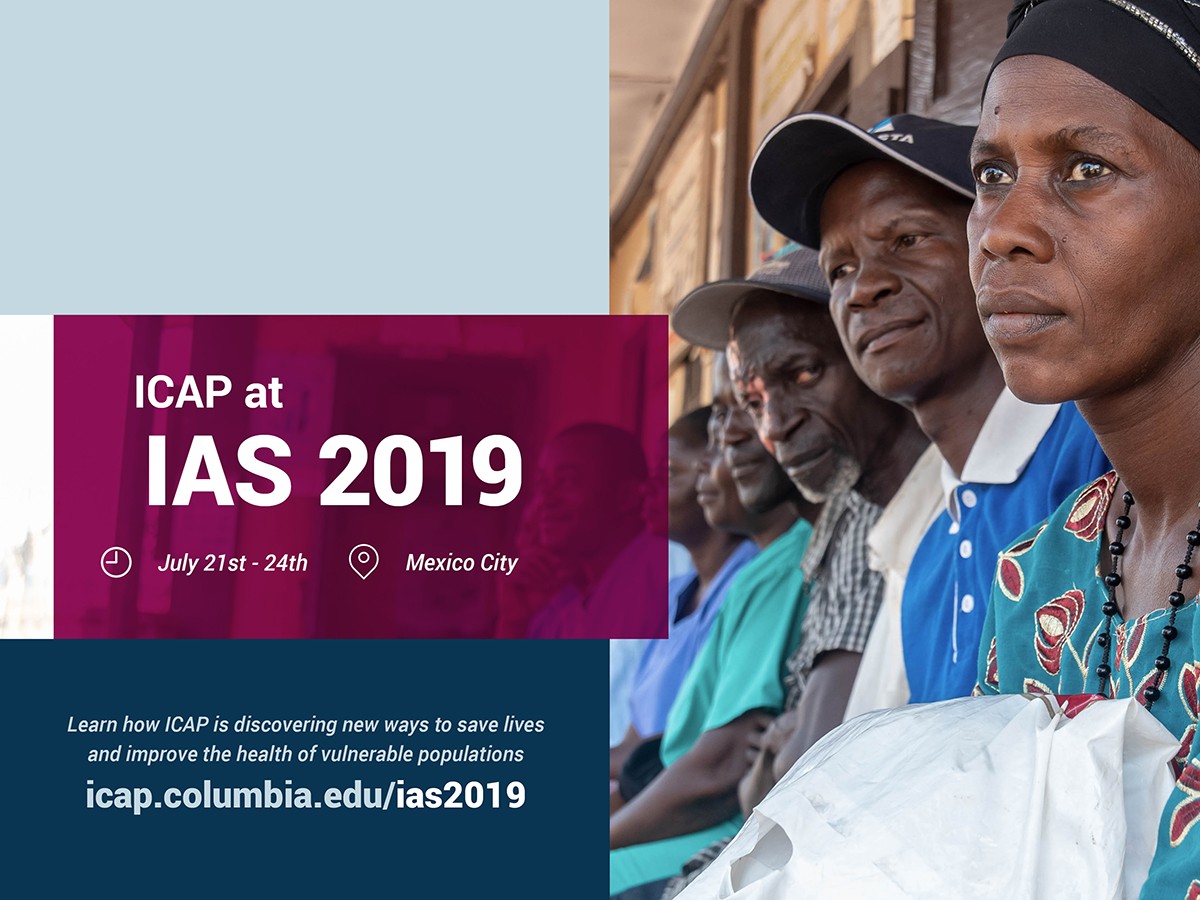
Date: July 21-24, 2019
-
Location: Centro Citibanamex, Mexico City
Click for conference information
Click for ICAP listings in online conference program
Jump to Conference Days:
Jump to Satellite Sessions:
- Saturday, July 20 (8:00 a.m. – 5:30 p.m.):
IAS TB/HIV 2019 Symposium: “A new era in TB prevention: Implications for People living with HIV” - Sunday, July 21 (8:00 – 10:00 a.m.):
“Sticky linkage”: Latest evidence and new strategies (SUSA01) - Sunday, July 21 (10:15 a.m. – 12:15 p.m.):
HIV recency testing to accelerate epidemic control: Early results and ethical considerations (SUSA05) - Sunday, July 21 (2:45 – 4:45 p.m.):
One year on: Updated WHO guidelines on first line treatment for people living with HIV (SUSA13) - Sunday, July 21 (5:00 – 7:00 p.m.):
Differentiated Service Delivery: Innovating to Address the Needs of People at High Risk of HIV Disease Progression (SUSA24) - Sunday, July 21 (5:00 – 7:00 p.m.):
2025 AIDS targets: Setting the next generation of goals for the global AIDS response (SUSA25) - Monday, July 22 (7:00 – 8:30 a.m.):
Launch of the Start Free Stay Free AIDS Free Report 2019 (MOSA08) - Monday, July 22 (7:00 – 8:30 a.m.):
Addressing the quality gap within HIV programmes: Improving clinical outcomes and preventing HIV drug resistance (MOSA01) - Monday, July 22 (6:30 – 8:30 p.m.):
Opportunity or threat: What is the implication of differentiated service delivery for TB/HIV services? (MOSA11) - Tuesday, July 23 (7:00 – 8:30 a.m.):
Eliminating HIV-related stigma and discrimination: Moving towards a global strategy (TUSA02)
Jump to Other Sessions:
- Tuesday, July 23 (1:00 – 2:00 p.m.):
Oral Poster Discussion Session: “Measuring, mapping and working with populations most in need” (TUPDD01) - Tuesday, July 23 (4:30 – 6:00 p.m.):
Oral Abstract Session: “Hot off the press: What’s new in HIV prevention” (TUAC04) - Tuesday, July 23 (5:00 – 6:00 p.m.):
IAS TB/HIV Cascades Stakeholder Meeting
Saturday, July 20 ▲
IAS TB/HIV 2019 Symposium: “A new era in TB prevention: Implications for People living with HIV.” ▲
Saturday, July 20, 8:00 a.m. – 5:30 p.m.
Hotel Camino Real Polanco, Mexico City
More information on the ICAP site
Full IAS TB/HIV symposium schedule
Andrea Howard, MD, MS, director of ICAP’s clinical and training unit, and Peter Preko, MBChB, MPH, CQUIN program director, will present at the IAS TB/HIV 2019 Symposium as part of IAS 2019 in Mexico City.
Dr. Howard’s presentation, “TB prevention in HIV-associated TB: opportunities and challenges,” will take place from 11:10 – 11:25 a.m. during “Session 3: Opportunities to scale up TB preventive treatment,” co-chaired by Vanessa Rouzier (GHESKIO, Haiti) and Kate Thomson (The Global Fund, Switzerland).
Dr. Preko’s presentation, “Use of differentiated service delivery approaches for TB prevention and care,” will take place from 1:50 – 2:05 p.m. during “Session 4: Field perspectives in scaling up TB preventive treatment among people living with HIV,” co-chaired by Sevim Ahmedov (USAID, USA) and Adeeba Kamarulzaman (University of Malaya, Malaysia).
The symposium is co-chaired by Dr. Alfredo Ponce de León (National Institute Salvador Zubirán in Mexico) and Dr. Beatriz Grinsztejn (Instituto National de Infectologia Evando Chagas-Fiocruz, Brazil and IAS Governing Council member).
Sunday, July 21 ▲
Satellite: “Sticky linkage”: Latest evidence and new strategies (SUSA01) ▲
Sunday, July 21, 8:00 – 10:00 a.m.
Palacio de Iturbide 1 y 2
http://programme.ias2019.org/Programme/Session/120
Organizer:
International AIDS Society
Co-Chairs:
Meg Doherty, World Health Organization, Switzerland
Getrude Ncube, Ministry of Health and Child Care, Zimbabwe
Summary:
What is needed to make linkage effective? How can we ensure our linkage approaches drive improved ART initiation and retention? How can we adapt these approaches for re-engagement of people who have been on treatment in the past but have fallen out of care? This session will address these questions through a differentiated service delivery lens. It will explore the term “sticky linkage” and its usefulness, the importance of global and country guidance on linkage and a minimum linkage service delivery package. Presentations will focus on filling gaps in the evidence base highlighting client-centered approaches. Presentations and debate will consider the importance of effective tracing approaches, the utility of compulsory adherence support upon re-entry and the need for clear country standard operating procedures on re-engagement to reduce delays in restarting treatment. The target audience for this session is policy makers, program implementers and implementation scientists.
Agenda:
PART 1: “STICKY LINKAGE” IN THE TREAT ALL ERA
- Opening framing on “sticky linkage”
Anna Grimsrud, International AIDS Society (IAS), South Africa
- Opening discussion
Kate Dovel, PIH, Malawi
Stella Kentutsi, NAFOPHANU, Uganda
PART 2: LATEST EVIDENCE AND NEW STRATEGIES
- A joint universal access point for couples in South Africa
Natasha Davies, Wits RHI, South Africa
- Peer providers to support from HIV self-testing to ART initiation in Burundi
Dismas Gashobotse, FHI 360, Burundi
- System redesign to improve linkage and ART initiation rates in Angola
Juliana Soares Linn, ICAP, United States
- Community-based service models to improve linkage to and retention in ART for female sex workers in Tanzania
Lung Vu, Population Council/Project SOAR, United States
- Segmentation of South Africa men – insights to improve linkage
Shawn Malone, PSI, South Africa
PART 3: REFRAMING FOR RE-ENGAGEMENT – BEYOND THE 90S
- Overview of re-engagement
Lynne Wilkinson, International AIDS Society (IAS), South Africa
- Lessons learned from South Africa’s Siyenza – “February Frenzy” to re-engage those cycling out or at risk of cycling out of care
Jonathan Grund, CDC, South Africa
- Who should be prioritized for re-engagement tracing?
Mpande Mukumbwa-Mwenechanya, CIDRZ, Zambia
Kimberly Green, PATH, Vietnam
Satellite: HIV recency testing to accelerate epidemic control: Early results and ethical considerations (SUSA05) ▲
Sunday, July 21, 10:15 a.m. – 12:15 p.m.
Casa Montejo 1
http://programme.ias2019.org/Programme/Session/55
Organizers:
ICAP at Columbia University and the University of California, San Francisco
Co-Chairs:
Jessica Justman, ICAP at Columbia University, United States
George Rutherford, University of California, San Francisco, United States
Summary:
As countries make strides towards universal diagnosis, treatment and viral suppression for people living with HIV (PLHIV), implementing strategies to identify new HIV cases and rapidly intervening to stop the chain of transmission will be critical. This satellite session will focus on updates from the field on rolling out the rapid test for HIV recent infection (RTRI) as part of the Tracking with Recency Assays to Control the Epidemic (TRACE) project. The session will feature speakers from Ethiopia, Malawi and Rwanda who will share early results on leveraging the new testing technology to identify geographical clusters of new infections and targeting prevention efforts to halt ongoing transmission. The session will consider ethical aspects of RTRI in order to ensure the rights of PLHIV are protected, and representatives from civil society organizations will discuss the important role they play in interpreting and using the recency data.
Presentations:
- Accelerating Epidemic Control with Recency
Ambassador Deborah Birx, US President’s Emergency Plan for AIDS Relief (PEPFAR), United States
- Laboratory validation of RTRI and field performance
Ernest Yufenyuy, Centers for Disease Control and Prevention
- Surveillance and Public Health Response using Recency: Early Evidence from the Field
Getachew Tollera, Deputy Director General, Ethiopian Public Health Institute (EPHI)
Placidie Mugwaneza, Rwanda Biomedical Center, MOH
Nguyen Hoang Long, Director, Vietnam Administration for AIDS Control
- Recent Infection Surveillance among Pregnant Adolescent Girls and Young Women in Malawi
Rose Nyirenda, Ministry of Health
- Panel Discussion on using recency data to benefit PLHIV, ethical considerations and program implications
Andrea Kim, Centers for Disease Control and Prevention (Moderator)
Amalia Girón, Universidad de la Valle, Guatemala
Rachel Baggaley, World Health Organization
Gregorio Millett, AmfAR
Wame Mosime, ITPC
Jerome Singh, University of KwaZulu-Natal
Satellite: One year on: Updated WHO guidelines on first line treatment for people living with HIV (SUSA13) ▲
Sunday, July 21, 2:45 – 4:45 p.m.
Palacio de Valparaíso 1
http://programme.ias2019.org/Programme/Session/154
Organizer:
WHO
Co-Chairs:
Elaine Abrams, ICAP at Columbia University, United States
Serge Eholie, Treichville University Teaching Hospital, Cote D’Ivoire
Summary:
WHO will present highlights from recent updates to the 2018 Interim Guidelines on first-line and second-line antiretroviral regimens. This satellite will review the current status of safety and efficacy of DTG based ARV regimens, including the basic science models, pregnancy cohorts, clinical trial evidence, risk benefit modelling and community values and preferences that fed into updated recommendations. WHO will share the most recent information on NNRTI pre-treatment resistance and implications for the use of DTG in first-line HIV treatment. The satellite will also share country policy uptake and implementation of DTG based regimens and explore how ministries have addressed the signal of NTD risk though a women’s center approach, integration of DTG use and SRH, and monitoring for side effects. A panel with representation from Ministries of Health, researchers, implementers and women living with HIV will review the implications of these new directions for HIV treatment programs.
Agenda:
Welcome by co-chairs
- Elaine Abrams, ICAP at Columbia University, United States
- Serge Eholie, Treichville University Teaching Hospital, Cote D’Ivoire
Presentations
- Directions from the updated WHO guidelines: the role of DTG for treating and preventing HIV infection – Opening remarks
Ren Minghui, WHO, Switzerland
- DTG based regimens in first- and second-line HIV treatment – updates to the WHO guidelines
Meg Doherty, WHO, Switzerland
- Review of what we know now about the signal of risk of neural tube defects with DTG use at conception
Lynne Mofenson, Independent Consultant, United States
- Modeling the benefits and harms of DTG use in pregnancy
Landon Myer, University of Cape Town, South Africa
- The role of pre-treatment NNRTI drug resistance and DTG use – evidence from the 2019 Global Report on HIVDR
Silvia Bertagnolio, WHO, Switzerland
Q&A
Panel Discussion: Implementation of DTG: How to scale up treatment, respect client choice and monitor for risk and integrate SRH – what we have learned in the last year and how to apply this to the years to come
Presentations
- Views from women seeking HIV treatment
Valeriia Rachynska, All Ukrainian Network of People Living with HIV/AIDS, Ukraine
- Views from Botswana’s country programme
Tendani Gaolathe, BCCP and Harvard-Botswana AIDS Initiative, Botswana
- Paediatric Treatment and care
Angela Mushavi, Zimbabwe Ministry of Health and Childcare, Zimbabwe
- Views on DTG use from Latin America
Trevor Peter, CHAI, United States
- How to improve access to DTG and SRH services
Imelda Mahaka, Pangea & AFROCAB, Zimbabwe
- PEPFAR remarks on TLD transition
Ambassador Deborah Birx, US President’s Emergency Plan for AIDS Relief (PEPFAR), United States
Q&A
Closing remarks
- Elaine Abrams, ICAP at Columbia University, United States
- Serge Eholie, Treichville University Teaching Hospital, Cote D’Ivoire
Satellite: Differentiated Service Delivery: Innovating to Address the Needs of People at High Risk of HIV Disease Progression (SUSA24) ▲
Sunday, July 21, 5:00 – 7:00 p.m.
Casa Montejo 1
http://programme.ias2019.org/Programme/Session/46
Organizer:
ICAP at Columbia University
Co-Chairs:
Jessica Justman, ICAP at Columbia University, United States
Tsitsi Apollo, Ministry of Health and Child Care, Zimbabwe
Summary:
Much progress has been made in designing efficient and people-centered Differentiated Service Delivery (DSD) treatment models for people with “stable” HIV who are doing well on ART. In contrast, there has been less innovation about service delivery for people with advanced HIV disease – who still comprise almost one-third of people initiating ART – and those at high risk of disease progression.
ICAP at Columbia University is a leader in the design, development, implementation and evaluation of HIV programs, working hand in hand with Ministries of Health (MOH) and diverse partners. ICAP’s HIV Coverage, Quality and Impact Network (CQUIN) brings countries together to share DSD innovations and to work together towards sustainable high quality HIV programs.
This satellite will convene implementers from MOH, civil society, implementing partners, donors and other stakeholders.
Presentations:
- Introductions & Framing Remarks
Jessica Justman, ICAP at Columbia University, United States
- The challenge of advanced HIV disease
Satvinder Singh, World Health Organization, Switzerland
- Differentiated Service Delivery models for people at high risk of HIV disease progression: a “call to action” from the CQUIN learning network
Peter O. Preko, ICAP at Columbia University, Eswatini
- The PEPFAR perspective
Catherine Godfrey, PEPFAR / Office of the Global AIDS Coordinator, United States
- Lessons from PHIA: Late diagnosis and partner risk
Andreas Haas, ICAP at Columbia University, Switzerland
- Tackling the procurement bottleneck to enable DSD models for people with advanced HIV disease
Carolyn Amole, Clinton Health Access Initiative (CHAI), United States
- DSD for people displaced by conflict: a perspective from South Sudan
Shambel Aragaw, ICAP at Columbia University, South Sudan
- DSD models for people at high risk of HIV disease progression: community perspective
Stella Kentutsi, NAFOPHANU, Uganda
2025 AIDS targets: Setting the next generation of goals for the global AIDS response (SUSA25) ▲
Sunday, July 21, 5:00 – 7:00 p.m.
Palacio de Iturbide 3
http://programme.ias2019.org/Programme/Session/49
Organizer:
UNAIDS
Chair:
Jose Antonio Izazola Licea, UNAIDS, Switzerland
Peter Godrey-Faussett, UNAIDS, Switzerland
Summary:
This session will aim to inform participants about the process that UNAIDS is leading to set targets for the global AIDS response post-2020. Although the session will focus on information sharing, participants will have an opportunity to contribute to the discussion and provide inputs.
ICAP founder and global director Wafaa El-Sadr, MD, MPH, MPA, will join Quarraisha Abdool Karim, PhD, and George Ayala, PsyD, in presenting outcomes and key considerations in setting targets from the Prevention, Treatment, and Social Enablers technical meetings. The session will be chaired by Shannon Hader, MD, MPH, deputy executive director of program for UNAIDS.
Presentations:
- Opening remarks
Shannon Hader, UNAIDS, Switzerland
- Keynote speaker: The response to HIV in the next decade
Ambassador Deborah Birx, U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), United States
- Outlining the deliverable of 2025 Targets process – and the potential influences
Adele Benzaken, Ministry of Health, Brazil
- Modeling the end of AIDS: Inside the black box – outline of the modeling approach
John Stover, Avenir Health, United States
- Outcomes of technical consultations in setting targets: Testing and Treatment
Wafaa El-Sadr, ICAP at Columbia University, United States
- Outcomes of technical consultations in setting targets: Primary Prevention
Quarraisha Abdool Karim, Columbia University/CAPRISA, South Africa
- Outcomes of technical consultations in setting targets: Social Enablers
George Ayala, MPact, United States
- Next steps and timeline
Jose Antonio Izazola Licea, UNAIDS, Switzerland
- Advocacy Needs as targets for the HIV response
Jorge Alejandro Saavedra Lopez, AHF, United States
- Government perspective on setting 2025 targets for HIV
Aleny Couto, Minister Of Health, Mozambique, Mozambique
- Closing Remarks
Peter Godfrey-Faussett, UNAIDS, Switzerland
Jose Antonio Izazola Licea, UNAIDS, Switzerland
Monday, July 22 ▲
Posters
Monday hours: 11:00 a.m. – 6:30 p.m.
Presentation hours: 12:30 – 2:30 p.m.
Sala B (Exhibition Level)
- High rates of viral load suppression among patients participating in home-based nurse-led ART adherence support intervention in Kazakhstan, Kyrgyzstan and Tajikistan (MOPEB262)
Presented by: Anna Deryabina
- Male partner age and HIV infection among young women in cohabitating partnerships in five countries in southern Africa (MOPEC344)
Presented by: Andrea Low
- Achieving the “third 90” in western Kenya: A Quality Improvement Collaborative (QIC) to improve viral load utilization at 30 health facilities in Siaya County, Kenya (MOPED538)
Presented by: Gillian Dougherty
- A Quality Improvement Collaborative (QIC) Approach to Improve Early Infant Diagnosis (EID) and Antiretroviral Therapy (ART) Initiation at 25 Health Facilities in Lusaka Urban District, Zambia (MOPED541)
Presented by: Gillian Dougherty
- Optimizing treatment models for people living with HIV in urban Zimbabwe: Findings from a mixed methods study (MOPED544)
Presented by: Jennifer Zech
- Systematic Review of the Evidence Regarding the Effectiveness of Community–Based Primary Health Care in Improving HIV/AIDS Outcomes for Mothers and Children (MOPED546)
Presented by: Ivy Mushamiri
- Reaching the last mile in Angola – Optimizing the HIV care cascade through intensified implementation support, the I-Surge (MOPED570)
Presented by: Juliana Soares Linn
- Patient feedback surveys about healthcare workers among women attending PMTCT services in eSwatini (MOPED612)
Presented by: Ilka Rondinelli
- Early results from Test and Start implementation in Luanda, Angola (MOPED633)
Presented by: Juliana Soares Linn
- Multi-Country Evaluation of Survival and HIV-Free Survival among Children under 3 Years of Age of Women Living with HIV in Eight Sub-Saharan African Countries: Results from Population-based HIV Impact Assessments (LBPEC21)
Presented by: Eugenie Poirot
Satellite: Launch of the Start Free Stay Free AIDS Free report 2019 (MOSA08) ▲
Monday, July 22, 7:00 – 8:30 a.m.
Palacio de Valparaíso 1
http://programme.ias2019.org/Programme/Session/170
Organizers:
UNAIDS, PEPFAR, EGPAF, ICAP at Columbia University, UNICEF, and WHO
Co-Chairs:
Ambassador Deborah Birx, U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), United States
Shannon Hader, UNAIDS, Switzerland
Summary:
Ambassador Deborah Birx, US Global AIDS Coordinator (PEPFAR) and Dr Shannon Hader, UNAIDS Deputy Executive Director, Programme will co-chair the launch of the Start Free Stay Free AIDS Free report 2019 – a global update of progress in access to HIV testing, prevention, treatment and care for children, adolescents and mothers and elimination of mother-to-child transmission of HIV. The main findings of the report will be presented and the co-chairs of each of the Start Free, Stay Free and AIDS Free technical working groups will present progress and challenges and highlight best practices. We will invite updates from the community and country perspective and conclude with a discussion on the key actions needed to accelerate progress towards the 2020 targets at country level and globally. The launch will serve as a rallying call to the international community to renew their strong commitment for concerted joint action to achieve the 2020 targets.
Presentations:
- Welcome and opening remarks from Chairs
- Overview of progress – Start Free Stay Free AIDS Free 2019 report
Shannon Hader, UNAIDS, Switzerland
- Community perspective
- Start Free – progress, challenges and best practices
Fatima Tsiouris, ICAP at Columbia University, United States
Alasdair Reid, UNAIDS, Switzerland
- Stay Free – Progress, challenges and best practices
Chewe Luo, UNICEF, United States
Janet Saul, CDC, United States
- AIDS Free – Progress, challenges and best practices
Meg Doherty, World Health Organization, Switzerland
Charles Lyons, Elizabeth Glazer Pediatric AIDS Foundation, United States
- Country perspectives
- Moderated discussion on country priority actions to accelerate towards the 2020 targets
- Conclusion and 2020 vision
Ambassador Deborah Birx, US President’s Emergency Plan for AIDS Relief (PEPFAR), United States
Satellite: Addressing the quality gap within HIV programmes: Improving clinical outcomes and preventing HIV drug resistance (MOSA01) ▲
Monday, July 22, 7:00 – 8:30 a.m.
Palacio de Iturbide 1 y 2
http://programme.ias2019.org/Programme/Session/160
Organizer:
World Health Organization
Co-Chairs:
Satvinder Singh, World Health Organization, Switzerland
Francois Kesner, Ministry of Health, Haiti
Summary:
This satellite will highlight the need to address quality gaps within HIV programs, share WHO guidance on strengthening quality of HIV services, country experiences in implementation of national quality strategies, and community perspectives on demand-side actions to support quality care.
Presentations:
- Why Quality Matters in ART Programmes
Charles Holmes, Georgetown University, United States
- Update on Global Progress in ART Outcomes: Need for a Quality Revolution
Silvia Bertagnolio, World Health Organization, Switzerland
- Quality Approaches to reach 90:90:90 and prevent HIVDR: the importance of national quality frameworks
Andrew Likaka, Quality Management and Digital Health, Ministry of Health, Malawi
- Panel Discussion: the essential components of improving quality of HIV service delivery, from collaboratives to quality systems
Solange Baptiste, International Treatment Preparedness Coalition, South Africa
Aleny Couto, Minister Of Health, Mozambique, Mozambique
Felipe Perini, Ministry of Health, Brazil
Judy Khanyola, ICAP, Columbia University, Kenya
Bruce Agins, University of California – San Francisco, United States
Satellite: Opportunity or threat: What is the implication of differentiated service delivery for TB/HIV services? (MOSA11) ▲
Monday, July 22, 6:30 – 8:30 p.m.
Casa Montejo 1
http://programme.ias2019.org/Programme/Session/45
Organizer:
ICAP at Columbia University
Co-Chairs:
Wafaa El-Sadr, ICAP at Columbia University
Vindi Singh, World Health Organization
Summary:
TB is the leading cause of death for people living with HIV, but TB prevention and treatment are lagging. As countries scale up HIV differentiated service delivery (DSD), there are important implications for TB/HIV services. Shifting recipients of care who are doing well on ART to less-intensive models is hoped to improve satisfaction, provider workload, and health system efficiency: it also means that many people on ART will be spending less time at health facilities. Appointment spacing and fast-track models require fewer and faster clinic visits. Other models will shift services to the community level. These changes create both challenges and opportunities for TB/HIV service delivery. Will these less-intensive models be able to provide effective TB screening and referrals? Can TPT be delivered safely to patients in community settings?
This satellite will convene participants from MOH, civil society, implementing partners, donors and other stakeholders.
Presentations:
- Introductions & Framing Remarks
Wafaa El-Sadr, ICAP at Columbia University, United States
- TB screening and differentiated service delivery: state of the art
Andrea Howard, ICAP at Columbia University, United States
- TB preventive treatment and differentiated service delivery: state of the art
Salome Charalambous, Aurum Institute, South Africa
- TB/HIV and DSD: the perspective from PEPFAR
Hank Tomlinson, U.S. Centers for Disease Control & Prevention, United States
- Highlights f