
HIV risk factors

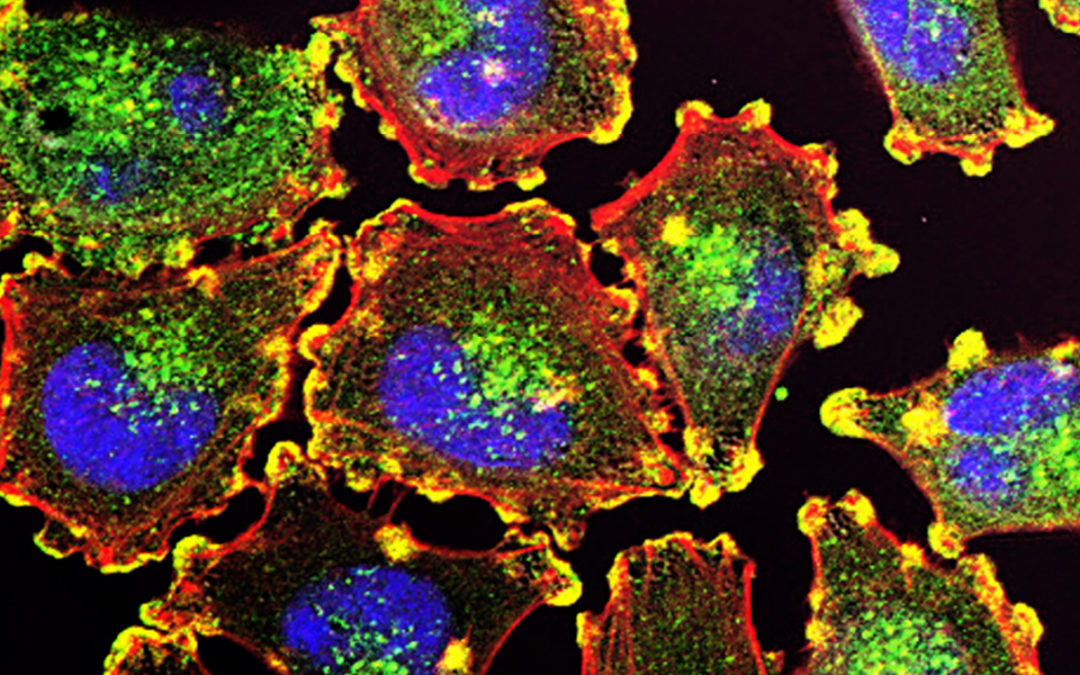
Risk for Non-AIDS-Defining and AIDS-Defining Cancer of Early Versus Delayed Initiation of Antiretroviral Therapy : A Multinational Prospective Cohort Study
Chammartin F, Lodi S, Logan R, Ryom L, Mocroft A, Kirk O, d’Arminio Monforte A, Reiss P, Phillips A, El-Sadr W, Hatleberg CI, Pradier C, Bonnet F, Law M, De Wit S, Sabin C, Lundgren JD, Bucher HC. Ann Intern Med. 2021 Mar 16. doi: 10.7326/M20-5226. Epub ahead...
Understanding HIV and Associated Risk Factors Among Religious Groups in Zimbabwe
Munyaradzi Mapingure, Zindoga Mukandavire, Innocent Chingombe, Diego Cuadros, Farirai Mutenherwa, Owen Mugurungi & Godfrey Musuka BMC Public Health (2021) doi: https://doi.org/10.1186/s12889-021-10405-8 Abstract Background The influence of religion and belief...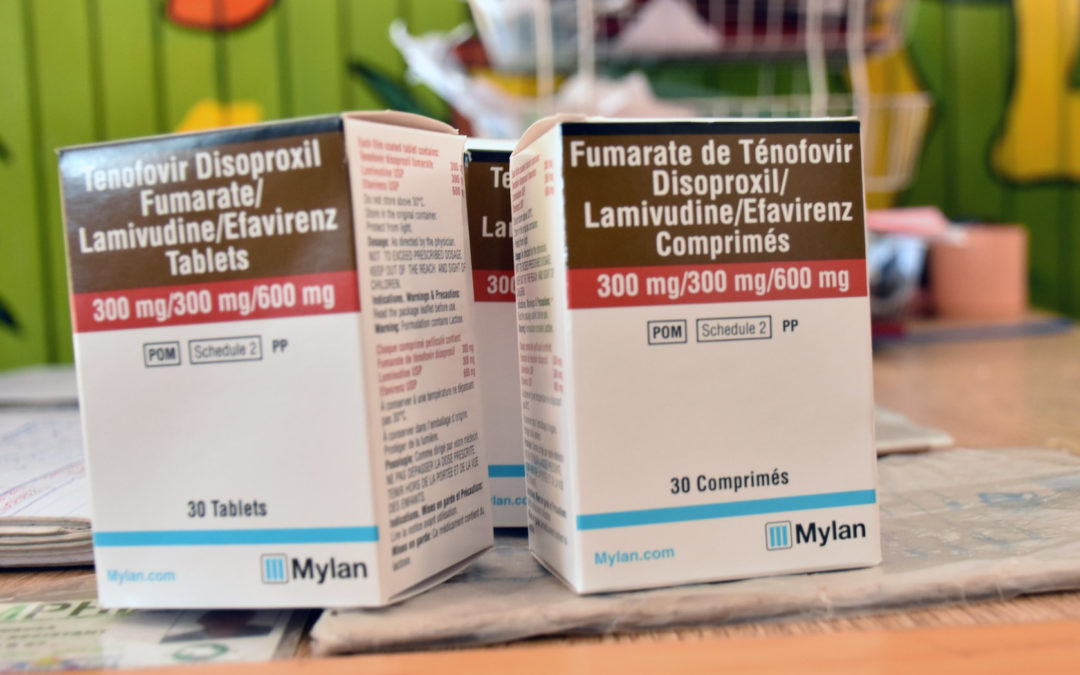
Optimizing differentiated treatment models for people living with HIV in urban Zimbabwe: Findings from a mixed methods study
Rabkin M, Strauss M, Mantell JE, Mapingure M, Masvawure TB, Lamb MR, et al. (2020) Optimizing differentiated treatment models for people living with HIV in urban Zimbabwe: Findings from a mixed methods study. PLoS ONE 15(1): e0228148....


