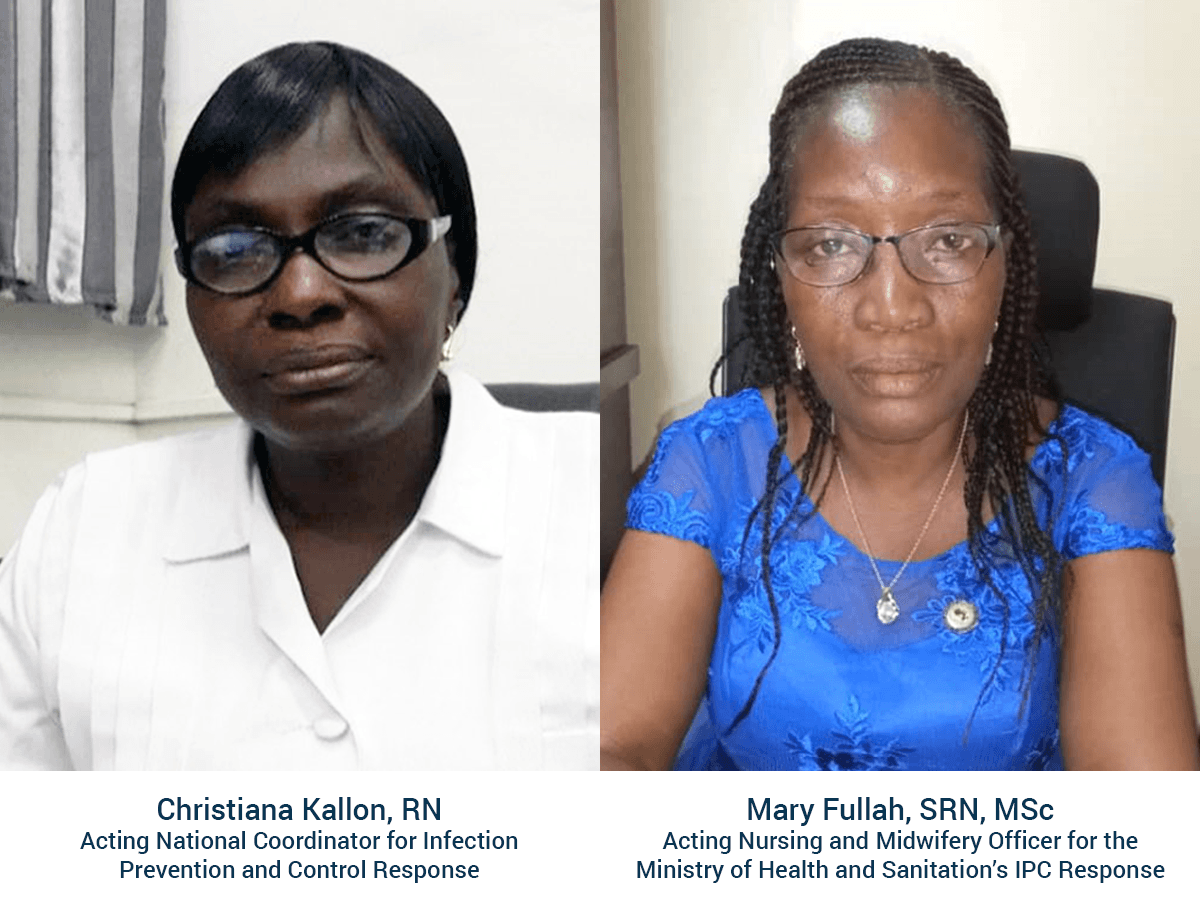
In this interview, Christiana Kallon, RN, acting national coordinator for infection prevention and control (IPC) response, and Mary Fullah, SRN, MSc, acting nursing and midwifery officer for the Ministry of Health and Sanitation’s IPC response, share their insights about the importance of IPC and how their work is creating a safer health care environment for patients and providers alike.
To read more about IPC efforts in Sierra Leone, Georgia, and Thailand, read the story here.
—
What does infection prevention and control (IPC) mean to you?
CK: IPC is an important component of our health care delivery system that aims to improve health outcomes, prevent future outbreaks, and establish a culture of safety in health care facilities.
MF: IPC is an essential element that helps eradicate and prevent cross-infections among health care providers, patients, hospitals visitors, and the community.
—
What are you doing in your specific role to advance IPC in Sierra Leone?
CK: In my role, I am in charge of coordinating IPC implementation throughout all of Sierra Leone, on behalf of the Ministry of Health and Sanitation. At the foundational level, we aim to establish IPC units in every hospital in the country, each with a designated IPC focal person. We also want to have an IPC link nurse in every hospital unit—for example, the maternity ward or the intensive care unit—and every primary health care facility. These staff will be supported at the district level by an IPC supervisor and district IPC focal person, to ensure coordination and quality, with quarterly IPC monitoring and supportive supervision from the national level. We also aim to create a three-year action plan to develop national IPC policy and guidelines, which will be condensed into pocket guidelines for health care workers. It is important that all health care workers, both clinical and non-clinical, receive training and supportive resources so that IPC can be implemented at every point of the health care system.
MF: Nurses and midwives are at the front lines of IPC because they are often the first point of contact for any patient, and they spend the most time with patients while they are in care. In Sierra Leone, we learned how important IPC training and practices were for frontline health workers during the Ebola epidemic, which claimed so many lives and put a big strain on the health system. To this end, we are focusing on raising awareness among health workers so they understand and apply IPC in all situations, and ensuring that supplies of IPC equipment, such as protective gloves, masks, and other items, are stocked and available to all health workers who need them. We are also providing supervision in health facilities to encourage both health workers and patients to practice IPC—for example, proper handwashing or using cough hygiene in waiting rooms. During the Ebola outbreak, we used house-to-house visits to share messaging about IPC in the community, which was effective in reducing the risk of disease transmission and increasing awareness about when to come to the health facility for diagnosis and treatment.
—
How has the MOHS partnership with ICAP helped you in your work?
CK: ICAP is one of the strongest supporting partners in IPC implementation in Sierra Leone, and they recently piloted a Rapid Improvement Model project for quality improvement in eight hospitals nationwide, focusing on three major IPC challenges: environmental cleanliness, waste management, and personal protective equipment. ICAP has also supported the development of a monitoring and evaluation framework, trained IPC officers on quality improvement methods, and worked with the national IPC unit to conduct quarterly monitoring and supportive supervision of activities at the hospital level. Right now, ICAP is supporting IPC curriculum development to improve and expand our trainings, including advanced IPC training so we can be ready in case of another crisis like Ebola. These activities will also help us improve our routine IPC practices to prevent and control health care-associated infections and antimicrobial resistance.
MF: One of the best IPC innovations ICAP has supported in Sierra Leone over the past year has been the development of a model ward at the Princess Christian Maternity Hospital, which is the main maternity hospital in Freetown and also the site of the National School of Midwifery. The capacity in the model ward was reduced from 21 to 15 beds in order for the staff to focus on providing the highest quality care, and IPC stations have been installed to hold gloves and other necessary supplies. Hospital staff and student midwives receive IPC training and supportive supervision to help them adhere to the highest standards of practice.
—
How have you seen these IPC efforts making a difference?
CK: The ongoing training for health care workers has increased knowledge of IPC practices and helped ensure a safe working environment for everyone, with lower risk of health care-associated infections. Additionally, the project has supported community sensitization and hand hygiene campaigns, which have resulted in increased awareness of IPC at the community level and revived the culture of hand-washing that helped eradicate Ebola.
MF: Community awareness of IPC has gradually grown, and hospitals have improved tremendously in the management and disposal of waste. They now hire qualified agents to clean the facilities and linens and dispose of hospital waste. Additionally, with ICAP’s provision of protective and cleaning equipment like waste bins, bin liners, gloves, sharps boxes, hand washing buckets, liquid soaps, and hand sanitizers, health care workers have been able to practice IPC methods and drastically reduce cross-infection among patients.
A global health leader since 2003, ICAP was founded at Columbia University with one overarching goal: to improve the health of families and communities. Together with its partners—ministries of health, large multilaterals, health care providers, and patients—ICAP strives for a world where health is available to all. To date, ICAP has addressed major public health challenges and the needs of local health systems through 6,000 sites across more than 30 countries. For more information about ICAP, visit: icap.columbia.edu
Photo caption—Header photo: Sign in Sierra Leone during the Ebola crisis of 2014-15.