 Resilience. Flexibility. Patience. These three traits are critical for anyone engaging in on-the-ground work related to global public health, whether it be through program or study implementation, monitoring and evaluation, or field epidemiology. On paper, anyone ambitious enough to want to go in the direction of global health thinks that they could handle moving to a completely different country for a short-term assignment and find a way to easily integrate themselves within that new community. This type of person has probably taken semesters of lectures on the impact of varying health challenges, and has read through stacks of policy reports and statistics, most likely viewing them as a proxy for understanding the real-life situation in their regions of interest. This person might think they are more than ready for a trip like this, and just anxious to start a new chapter. It’s a person like this who may overestimate their flexibility – who steps off the plane and the reality of working abroad hits them like a brick wall.
Resilience. Flexibility. Patience. These three traits are critical for anyone engaging in on-the-ground work related to global public health, whether it be through program or study implementation, monitoring and evaluation, or field epidemiology. On paper, anyone ambitious enough to want to go in the direction of global health thinks that they could handle moving to a completely different country for a short-term assignment and find a way to easily integrate themselves within that new community. This type of person has probably taken semesters of lectures on the impact of varying health challenges, and has read through stacks of policy reports and statistics, most likely viewing them as a proxy for understanding the real-life situation in their regions of interest. This person might think they are more than ready for a trip like this, and just anxious to start a new chapter. It’s a person like this who may overestimate their flexibility – who steps off the plane and the reality of working abroad hits them like a brick wall.
That’s what happened with me, at least.
Embarking on my journey as a Next Gen intern, I had an overall goal of contributing to decolonizing global health and working towards health equity and health systems autonomy. I would be lying if I said the first month of adapting to being in Eswatini – the focal point country of my practicum – was seamless. In retrospect, however, I think that month allowed me to self-examine whether I was adhering to my original goals, or if I was somehow using them as a pretense for a more selfish desire, which was to show that I really knew what it meant to work in global health and empower the local health system to provide care.
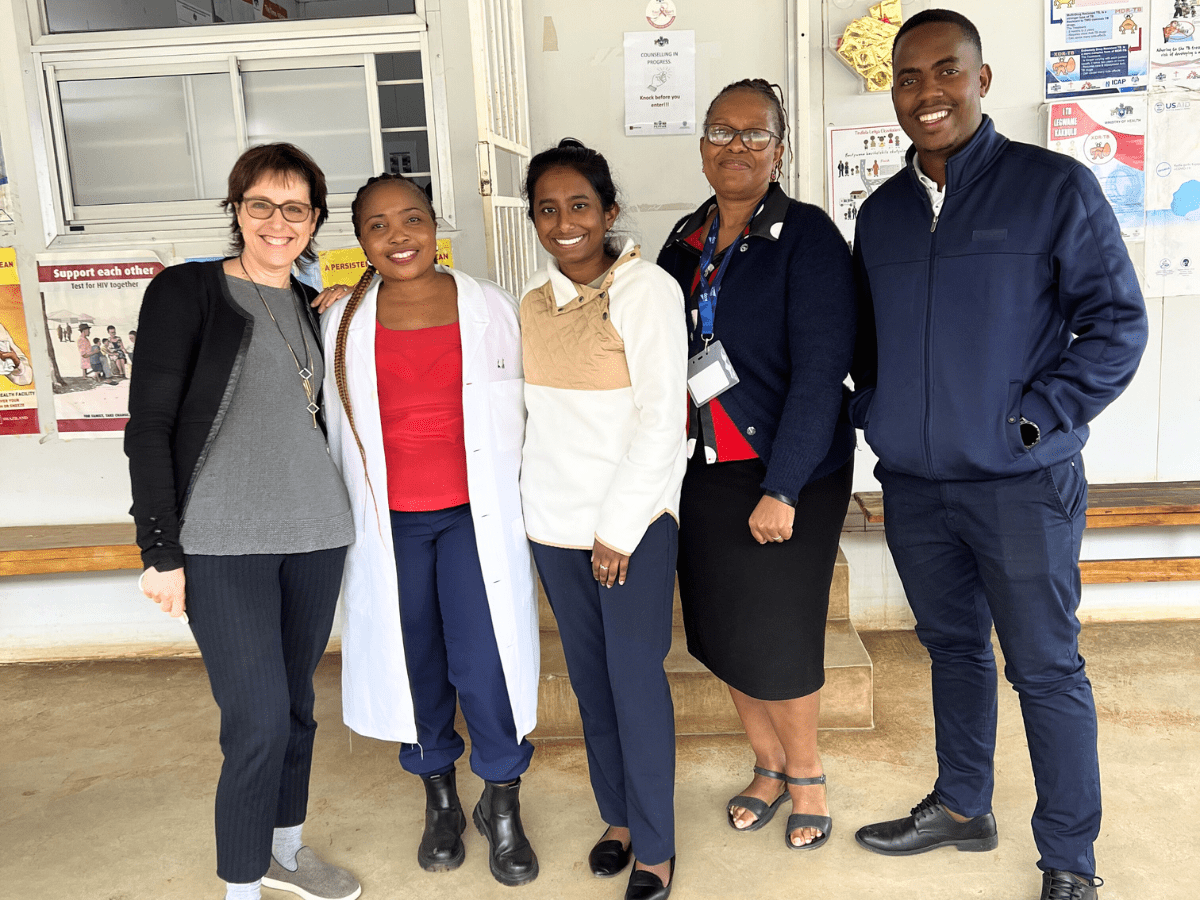
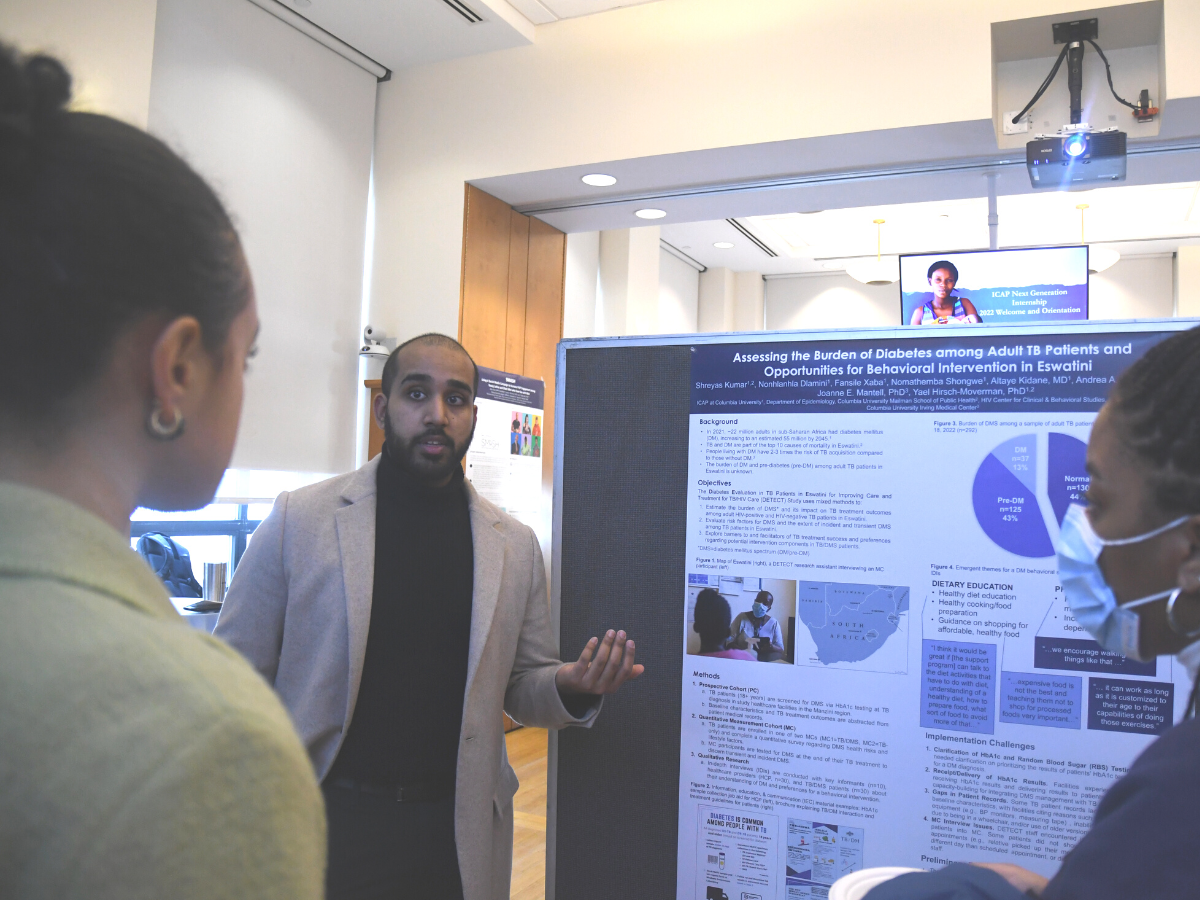
For about six months, I joined the ICAP in Eswatini team as part of the Diabetes Evaluation for TB Patients in Eswatini for Improving Care and Treatment in TB/HIV Care (DETECT) Study. My role was to support the implementation of the study in its initial phase, assist the in-country team through tool development and other technical support, and help identify and tackle any challenges along the way. We worked with ten health facilities in the Manzini region to mentor providers on screening TB patients for diabetes upon their initial TB diagnosis, ensuring that those samples were sent correctly to the central government laboratory in Mbabane, the administrative capital, for testing. Once those test results were provided back to the facilities to deliver to the patients, we would recruit these patients to partake in a quantitative survey about their understanding of diabetes. Some of those patients participated in a qualitative in-depth interview to provide insights on potential intervention components to manage and prevent diabetes.
During that first month, I would drive along with the study team as we went from clinics based in the bustling city of Manzini to those only accessible by a bumpy dirt path. With each visit and within discussion with nurse matrons at each site – which were often translated from siSwati for me by my supervisor – I realized how difficult implementing a study like this would be and I quickly became frustrated. We did not have any preliminary results yet, and I began to feel discouraged. It even reached a point where I completely forgot about my core goals and why I wanted to be there in the first place. However, it took a few conversations with my peers working in the other country offices around sub-Saharan Africa and with my principal investigator to ease this tension.
I needed to remember that waves of new challenges to implementation rise constantly and that the initial course of action in a project will not always be the course we stay on – that being frustrated that the study is not going the way it should be does absolutely nothing to solve the problems in real time. I needed to take a breath and ask, “How do we move forward?” and begin brainstorming new ideas. We tried to work with the barriers. At the end of the day, I realized this program was not necessarily about what I could accomplish; it was about working to ensure people with TB in Eswatini understood their diabetes status, which, if undiagnosed or untreated, would adversely affect the outcome of their TB treatment.
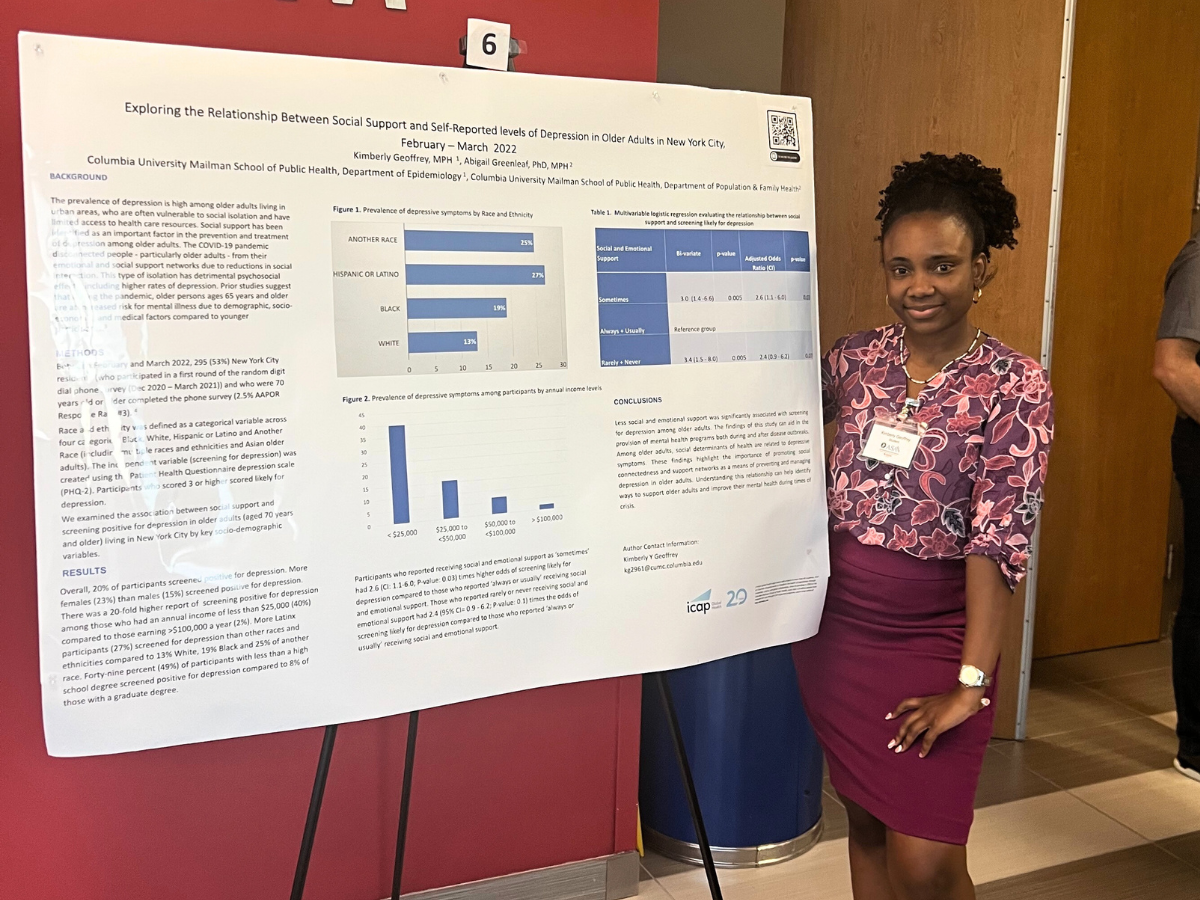
Not long after this reflection on patience, we received our preliminary results on the prevalence of diabetes among TB patients, which provided me with a foundation to continue understanding this burden and identify steps the Ministry of Health could take to intervene and manage this comorbidity. After that first month, I developed visual aids to support health care providers and patients to better understand the relationship between diabetes and TB, interviewed health care providers about their understanding of diabetes screening, management, and potential interventions, and even assisted in presenting our findings to regional stakeholders and implementing partners.
Looking back, I am grateful for that time in Eswatini, for my teammates and colleagues, for the experiences I would have never gotten if I were to be stuck in a classroom reading papers without knowing what that information I was reading really translates to in real life.
Shreyas Kumar
MPH Candidate in Epidemiology, Global Health Certificate
Mailman School of Public Health