In the heart of Eswatini (the country formerly known as Swaziland), women are being greeted by a new face as they arrive for their family planning, antenatal, or well-child visits. Long a staple at HIV clinics, “cough officers”—non-medical staff who screen patients for tuberculosis (TB) and navigate them through health services—are now part of routine care for women.
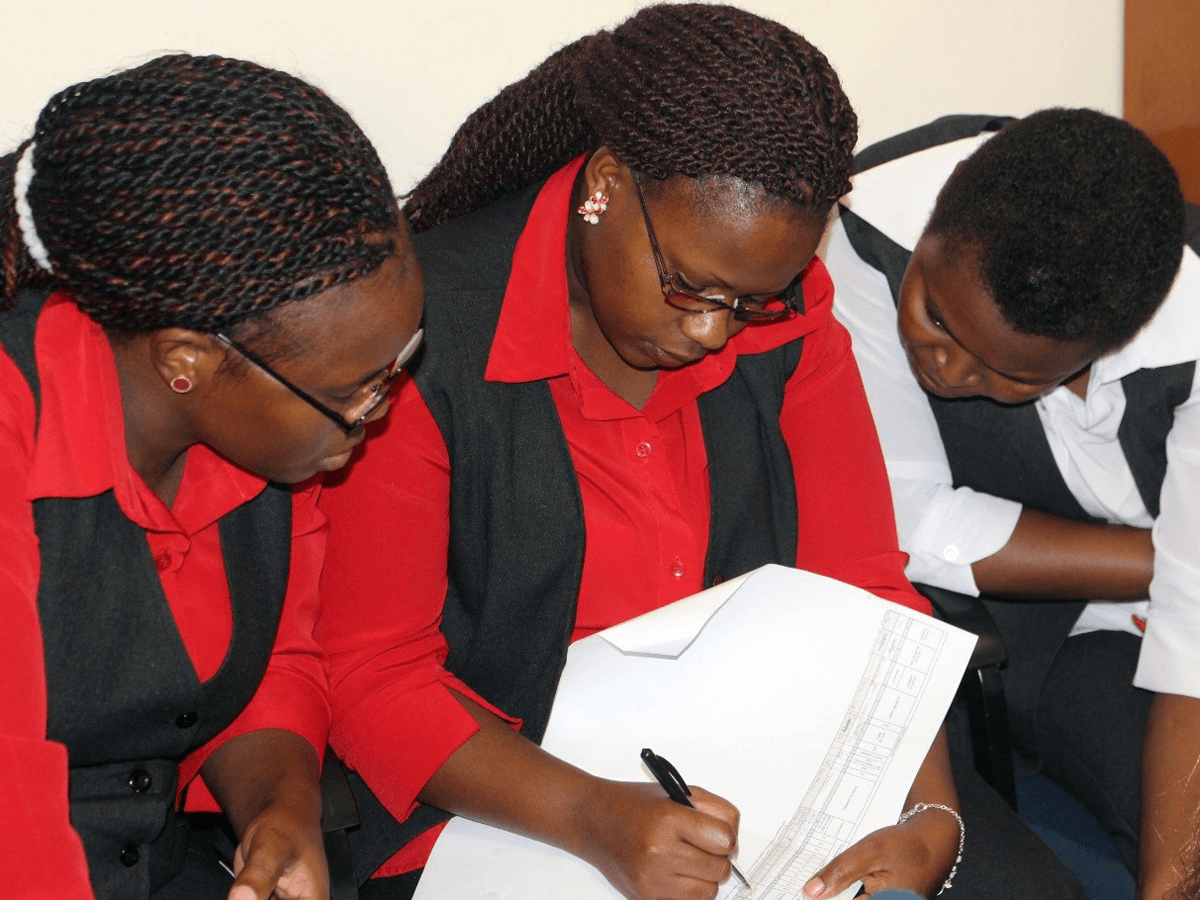
This potentially lifesaving innovation is part of a project led by ICAP in collaboration with the Reproductive, Maternal, Newborn, and Child Health (RMNCH) units at four health centers in the country’s Manzini Region. In adding TB services to routine care, these units are expanding their highly successful “one-stop-shop” model, which simplifies and expedites services to reduce waiting times and improve patient outcomes. A total of 71 health care workers received training to support the new procedures and patient flows, which are already producing good results.
“We’ve seen good, desirable outcomes at the end of TB treatment because of the one-stop-shop approach,” said one health care worker who was surveyed. “It helps that services are provided in one room, instead of referring our clients [to a different health facility].”
In Eswatini, HIV testing, care, and treatment have already been successfully integrated with women’s health services as the standard of care—essential in a country where more than one-third of women between 15–49 years of age are living with HIV.
Eswatini also has a high burden of TB, which is the deadliest opportunistic infection for people living with HIV, accounting for two out of every five AIDS-related deaths globally. In Eswatini, approximately 70 percent of the TB patients who know their HIV status are HIV positive.
For this project, ICAP worked with the Eswatini Ministry of Health and its National Tuberculosis Control Program to integrate TB screening, prevention, treatment, and contact tracing into RMNCH care, based on a new TB/HIV toolkit in development by the World Health Organization. Increasing the coverage and quality of both HIV and TB services has been a key focus of ICAP’s work in Eswatini, which is supported by the U.S. Centers for Disease Control and Prevention (CDC) with funding from the President’s Emergency Plan for AIDS Relief (PEPFAR).
“Awareness of HIV and TB in the community, including symptoms to watch for and how and where to get tested, has been improving over time—but nearly every woman knows about seeking services for family planning, antenatal care, and pediatric checkups. So this is a good opportunity to integrate TB services for the women and children who attend the clinic, and to initiate contact tracing for women diagnosed with TB, through local community-based organizations when necessary,” said Arnold Mafukidze, MBChB, MSc, the senior associate technical director for TB/HIV for ICAP in Eswatini. “Additionally, women appreciate being able to receive multiple services under one roof, since they are busy and sometimes travel quite far to receive care.”
Introducing the cough officer and adjusting patient flow was the first step. The cough officer now screens all incoming patients arriving in the unit using a special tool designed to identify TB in pregnant and breastfeeding women and their children.
Ensuring the health and safety of all patients is the top priority, so infection prevention and control measures have been introduced. Cough officers ensure all windows are open to maximize natural ventilation, triage all women with presumptive or active TB at the waiting areas, counsel them about cough etiquette, separate them where possible, and fast-track them through services to minimize the chance of transmitting infection to other patients.
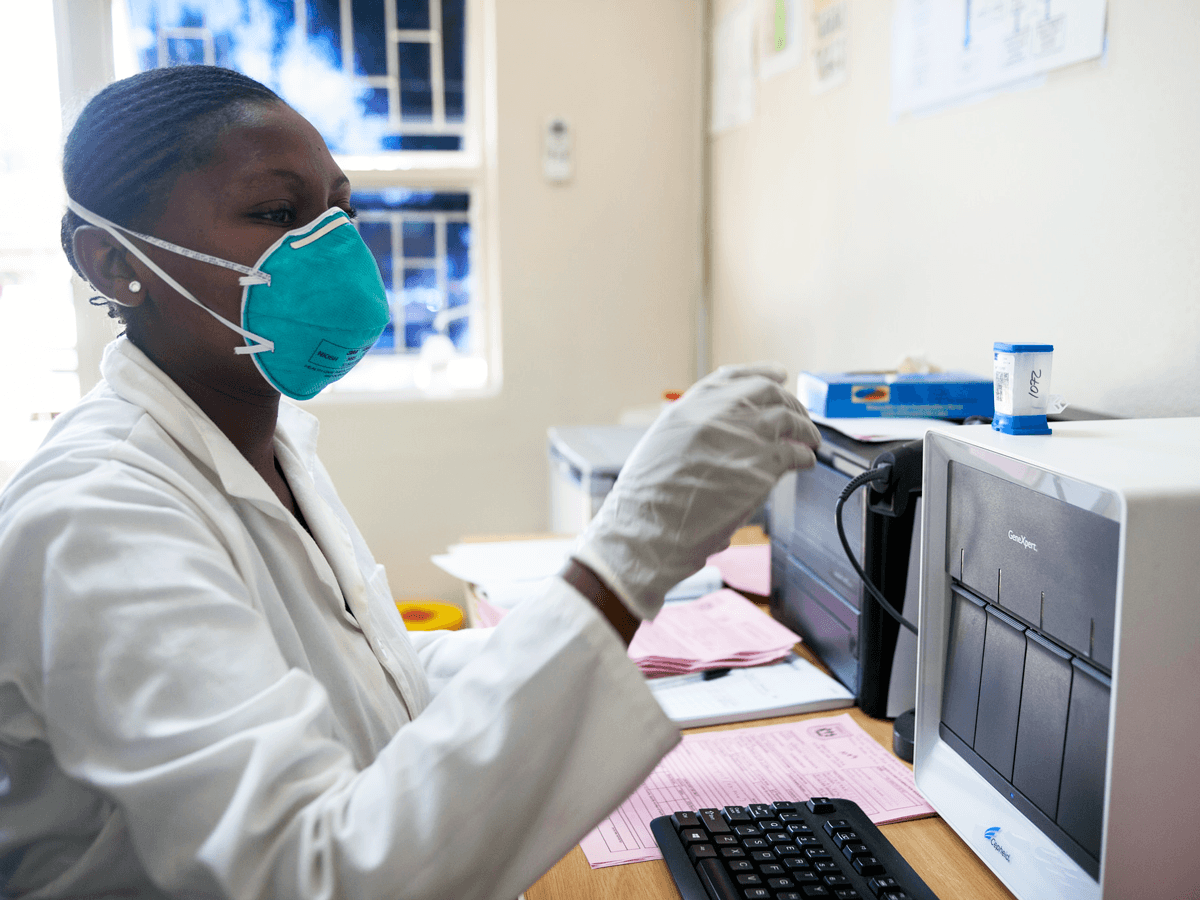
If screening indicates that a patient may have TB, the cough officer collects sputum samples and sends them to lab for testing while the patient is fast-tracked through the other services she has scheduled in the clinic.
If the tests confirm a positive TB case, the cough officer escorts the patient to the TB clinic to start treatment right away. Any patients who are HIV positive and screen negative for TB are offered a six-month course of Tuberculosis Preventive Therapy (TPT) to protect against the disease.
“TPT has been fully integrated into these services for women, leading to an increase in the numbers of women of reproductive age receiving the therapy,” said Phumzile Dlamini, MA, the TB/RMNCH integration nurse specialist for ICAP in Eswatini. “As a result, initiation of the therapy at ICAP project sites is nearly three times higher than the national average within HIV care and treatment settings.”
As part of integrating TB/HIV services, ICAP has also supported the four health facilities in introducing patient registers specifically adapted to record information about TB screening and services in a maternal and child health context. This information helps with national disease surveillance, and also enables contact tracing and follow-up.
Since few patients are able to bring their contacts to the clinic for screening, due to travel costs or competing priorities, ICAP works with community-based partners to provide supportive home visits for contact screening and referral to local health facilities.
“We actually see many antenatal care and breastfeeding clients who are only ‘visitors’ in the facility and receive their regular care elsewhere, so the outcome information in the RMNCH TB Register includes this information so they are not simply marked as ‘lost to follow-up,’” said Sister Nonhlanhla Mayimbela, BSN, sister-in-charge of the RMNCH unit at the Raleigh Fitkin Memorial Hospital.
Thanks to the concerted efforts and commitment of staff across the four facilities, this project is poised to have a lasting impact on TB prevention and treatment in Eswatini. Having demonstrated that integration of TB services into RMNCH care is both feasible and worth the extra effort, all four facilities have adopted the new TB procedures as part of routine care for all patients. Looking ahead, health care workers will continue to use the adapted TB screening tools and registers to improve case finding and patient management, and advocate for improvements to the national health information system to integrate TB data that can help save lives.
A global health leader since 2003, ICAP was founded at Columbia University with one overarching goal: to improve the health of families and communities. Together with its partners—ministries of health, large multilaterals, health care providers, and patients—ICAP strives for a world where health is available to all. To date, ICAP has addressed major public health challenges and the needs of local health systems through 6,000 sites across 30 countries. For more information about ICAP, visit: icap.columbia.edu
Photo captions—Header image: a lab technician runs a GeneXpert machine for rapid TB testing. Middle image: nurses at the Mankayane clinic in Eswatini receive training on the adapted TB registers.