Malaria is a leading health threat in Ethiopia, where more than two-thirds of the population lives in high-risk areas. It is the leading cause of outpatient visits and is a particularly deadly disease for children under five years of age and pregnant women.
Hospitals and health centers in Ethiopia primarily use microscopy to diagnose malaria; however, assuring the quality of this testing has been a longstanding challenge. As a result, clinicians have largely treated patients with suspected malaria empirically, despite a negative laboratory test due to unreliability of the results. This leads to overuse of antimalarial drugs in some situations and delay in specific treatment for other causes of fever.
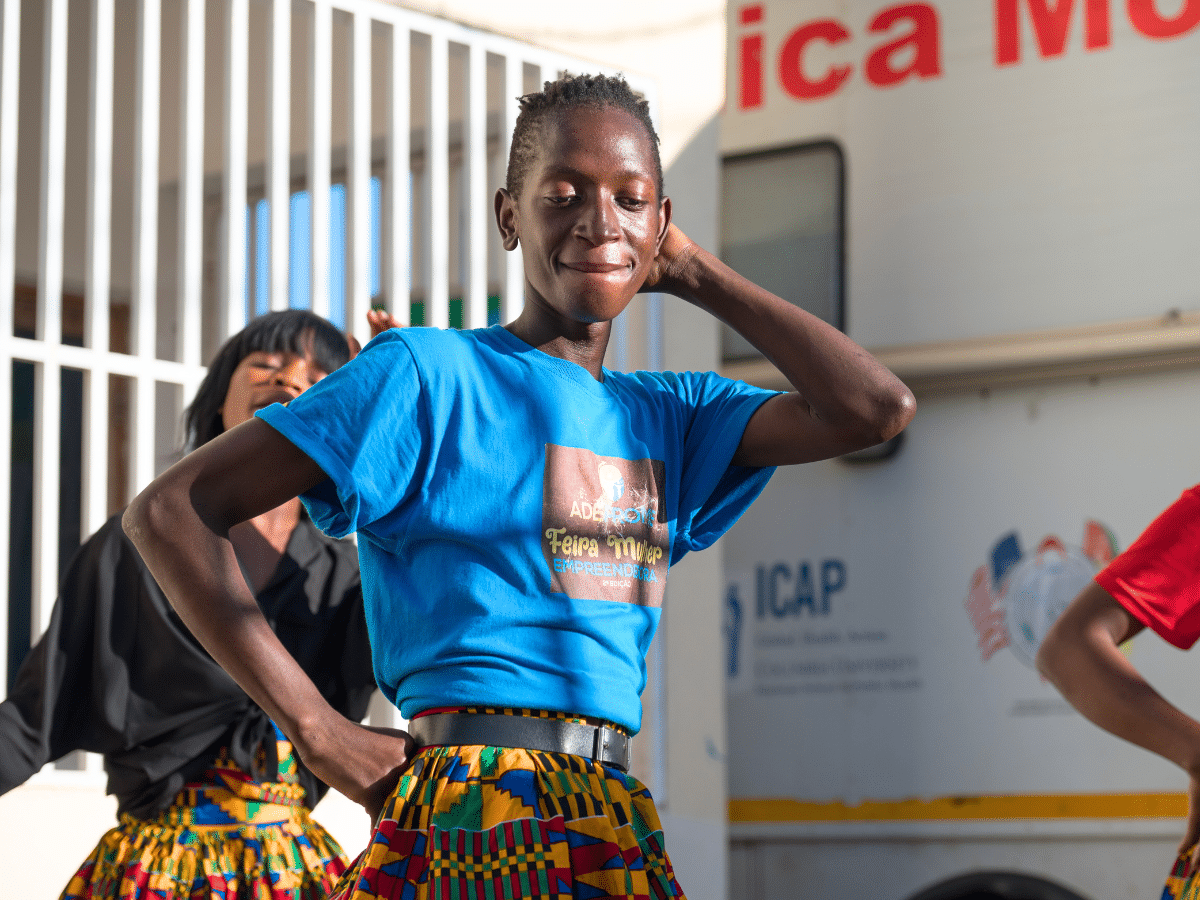
The President’s Malaria Initiative (PMI), led by USAID, is focused on reducing the burden of malaria in 19 sub-Saharan African countries. To meet Ethiopia’s ambitious goal of reducing malaria deaths by 70%, ICAP has worked for the past six years with PMI and the Federal Ministry of Health (FMOH) in Ethiopia to strengthen laboratory diagnostic capacity and malaria case management at the national, regional and health facility levels.
An initial survey, conducted by ICAP, of the national program, health centers and specialized laboratories revealed that most lacked adequate microscopes and had no standardized training programs for lab technicians. Only 24% of laboratory staff at these health facilities had received training in the previous year. In Addition, none of the laboratories surveyed had formal quality assurance (QA) or quality control protocols. There were also no standard national malaria diagnostic guidelines or national malaria laboratory quality assurance guidelines.
Starting in the Oromia Region, ICAP clinical and laboratory advisors began an intensive effort to partner with hospitals, health centers, clinics, and laboratories to provide targeted training and capacity building in malaria diagnosis for laboratory professionals. A national training manual for malaria microscopy was developed, as well as an external quality assurance guideline for malaria lab diagnosis.
Mr. Gemechis Mesfin, who directs laboratory services at Nedjo Hospital in Oromia, acknowledges, “We never knew anything about EQA—external quality assurance—activities before this training.”
In 2011, ICAP expanded it malaria-focused work to Ethiopia’s Amhara, Tigray and SNNPR regions, expanding support from 57 to 371 health facilities. Of these, eight regional laboratories were strengthened through training in malaria microscopy and equipped with new microscopes, reagents, standardized microscopic slides, and other essential laboratory commodities. Over 150 professionals from regional and national reference laboratories took part in ICAP’s initial training-of-trainers program in malaria microscopy and quality assurance. Further in-service training was then rolled out to an additional 1,400 laboratory personnel by the end of March 2014. This included a basic introduction to malaria/HIV laboratory diagnosis and practical skills, such as blood sample collection, smear preparation, staining, blood film examination, microscope maintenance, and HIV testing methods. A package of ICAP-developed resources, including the Malaria QA guidelines, standard operating procedures, job aides, bench aides and log sheets were provided to help standardize the quality of services and improve information management.
In addition to building laboratory capacity, ICAP developed an algorithm for managing fever and malaria patients and trained more 1,300 clinicians and program managers in its use, advancing one of the goals of the National Strategic Plan for Malaria—to treat all confirmed malaria cases with appropriate antimalarial drugs and manage all severe cases according to the new treatment guidelines.
With this intensive investment of resources in malaria, 80% of all clinically suspected diagnoses of malaria are now laboratory confirmed in Ethiopia. In Oromia, where ICAP began its malaria-focused work, substantial gains have been made in reducing presumptive treatment of malaria from 99% in 2007 to 23% in 2013. Stronger national standards for quality control also have led to improved test accuracy, which reduces the misdiagnosis of malaria and unnecessary use of antimalarial drugs.
With PMI’s support, ICAP is working with its partners to bring Ethiopia closer to the goal of zero malaria deaths.