ICAP at Columbia University is testing a theory: can a smartphone app help facilitate HIV self-testing and improve PrEP adherence?
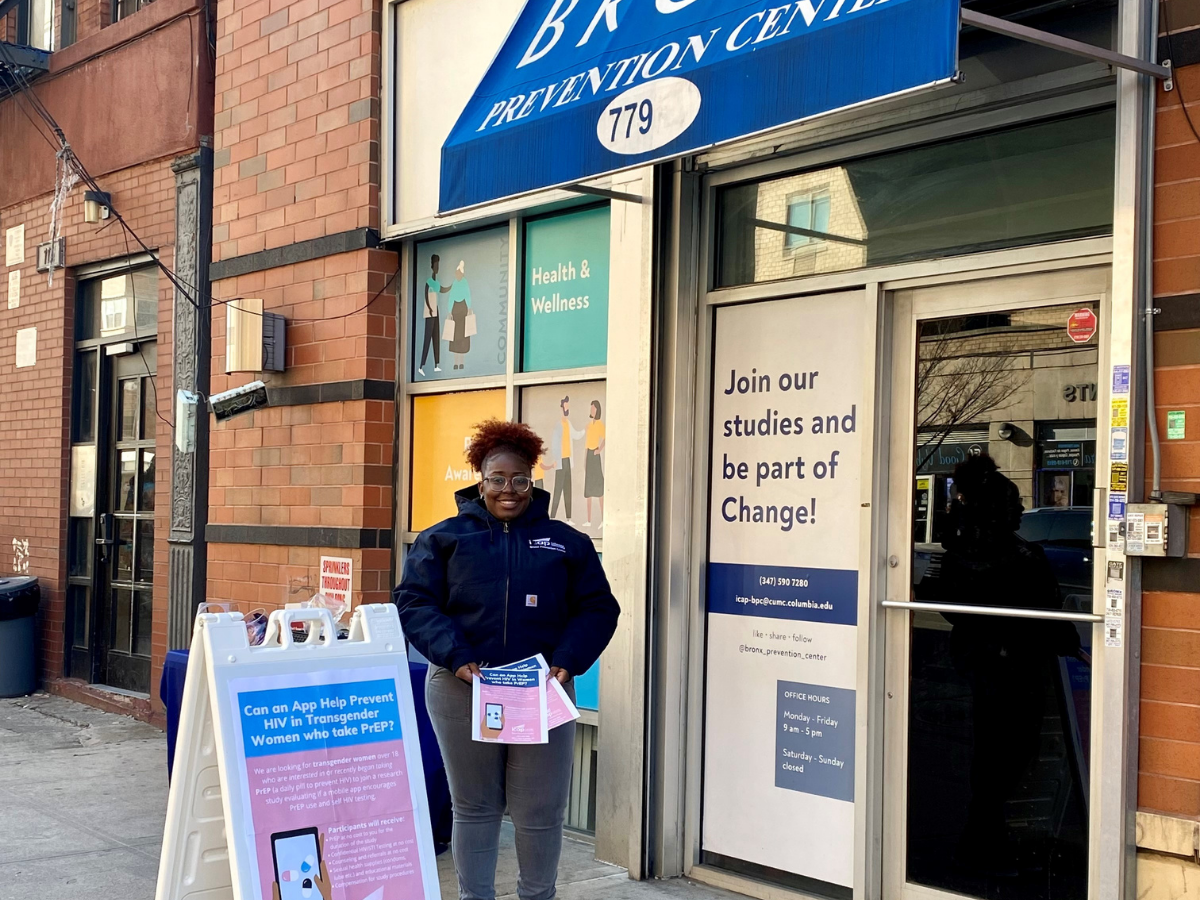
Beginning in January 2021, ICAP’s Bronx Prevention Center launched “Making PrEP Smart,” a study exploring the acceptability of an app designed to support adherence to pre-exposure prophylaxis (PrEP) and promote HIV self-testing and partner-testing. In contrast to other studies which have assessed apps supporting PrEP adherence among men who have sex with men, this study will enroll both cis- and transgender women.
PrEP – a highly effective medication regimen that, when taken daily, prevents people at risk for HIV from getting infected through sex or injection drug use – is underutilized by women. A 2018 study found that only 7 percent of women eligible for PrEP were using it. PrEP has been similarly underutilized among transwomen.
The mobile-phone app – SmartPrEP – was developed by Sam Sia, professor of biomedical engineering at Columbia University. The app provides reminders about taking PrEP and about self- and partner-testing, as well as assistance with interpreting test results and locating nearby clinics. The Making PrEP Smart study will assess the acceptability of the app, elicit user feedback on app features, and evaluate whether PrEP adherence and HIV testing frequency change with use of the app.
“Mobile apps have the potential to help patients, but they must be usable for the intended population,” said Sia. “We are working with ICAP colleagues to build an app that has the functionality and scalability to significantly impact the behavior and health outcomes of patients on HIV prophylaxis medication.”
“Assessing the acceptability of the app is important, for example, knowing whether it is cumbersome or difficult to use,” added Ann Kahn, MPH, MSN, senior site clinician at Bronx Prevention Center and lead clinician of the study. “That feedback could be used to modify the app. I know that many people use alarms on their phones to remind them to take medication. Will this app be a useful tool, and will it be an improvement over other ‘reminder’ methods?”
One of the major gaps the study aims to address is inconsistent PrEP usage, as the medication must be taken daily to be as effective as possible. In other studies conducted at the Bronx Prevention Center, participants have reported difficulties in taking pills every day due to lack of daily routines, unstable housing conditions, or simply forgetting to take the medication. While additional studies are investigating long-acting methods of PrEP, the daily pill currently remains the most accessible option.
“As we all integrate more and more technology into our everyday lives, it’s necessary to investigate how mobile health technology can be leveraged to support healthy behaviors,” said Connor Wright, MPH, senior project officer at ICAP and coordinator of the study. “Since the roll-out of PrEP in the U.S., there have been reports of low uptake and sub-par adherence, generally evaluated among men who have sex with men. New technologies, like the SmartPrEP app, have the potential to facilitate a wide range of preventative behaviors right from the palm of your hand. A smartphone app that supports these behaviors could prove to be a particularly useful strategy to increase PrEP uptake and regimen continuation among cisgender and transgender women, while also reducing the burden on patients and providers of frequent clinic-based follow-up.”
Participants of the study will download the app, then attend visits at the Bronx Prevention Center over a 12-month period for adherence counseling, app acceptability assessments, and behavioral risk assessments, as well as STI and HIV testing conducted according to CDC guidelines. Participants will also be invited to take part in either a focus group discussion or an open-ended, in-depth interview to elicit their thoughts and preferences on the app.
“HIV testing and medications like PrEP are crucial tools for addressing the HIV epidemic; however, those tools can only be leveraged if they are accessible and maintained,” said Jessica Justman, MD, senior technical director of ICAP and lead investigator of the study. “Given that an app like this has yet to be assessed among cis- and transgender women, this study will help us learn more about the potential of mobile health for HIV prevention of these populations. We especially want to know if combined services – like PrEP adherence support blended with HIV testing support – might lead to better outcomes for individuals at elevated risk of acquiring HIV.”
About ICAP
A major global health organization that has been improving public health in countries around the world for nearly two decades, ICAP works to transform the health of populations through innovation, science, and global collaboration. Based at Columbia Mailman School of Public Health, ICAP has projects in more than 30 countries and is working side-by-side with ministries of health and local governmental, non-governmental, academic, and community partners to confront some of the world’s greatest health challenges. Through evidence-informed programs, meaningful research, tailored technical assistance, effective training and education programs, and rigorous surveillance to measure and evaluate the impact of public health interventions, ICAP aims to realize a global vision of healthy people, empowered communities, and thriving societies. Online at icap.columbia.edu