Recognizing that antiretroviral therapy (ART) “keeps people living with HIV alive, healthier and reduces the risk of transmitting the virus to partners,” the World Health Organization in 2015 recommended that anyone infected with HIV should begin ART as soon after diagnosis as possible, rather than basing the decision on CD4 count or disease stage—an approach known as “Treat All.”
Expanded use of ART has had a huge impact: according to a UNAIDS/WHO report, more than 18 million people were receiving ART by mid-2016, and the global number of people dying from HIV-related causes had fallen by 45 percent since 2005. These gains are essential as the world strives to reach the UNAIDS 90-90-90 targets by 2020 and 95-95-95 by 2030.
Responding to interest from countries seeking to implement the Treat All approach and also increase national HIV testing coverage and yield, ICAP launched a compendium of “Test and Treat All” resources encompassing:
- Targeted HIV Testing
- Starting Antiretroviral Therapy in the Era of Treat All
- Differentiated Service Delivery
- Implementation of Routine Viral Load Monitoring
Now complete with its final installment in August 2018, this four-part package is a key part of ICAP’s portfolio of innovative tools to promote progress toward epidemic control.
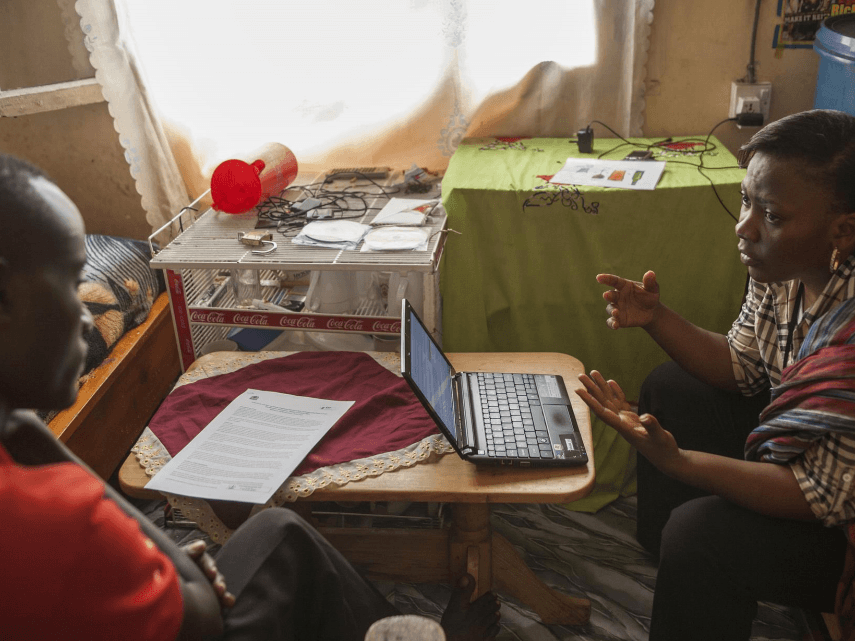
“These resources will assist countries in designing and rolling out programs to increase targeted HIV testing, improve ART coverage and retention in care, and maximize services to ensure viral load suppression,” said Andrea Howard, MD, MS, director of ICAP’s Clinical and Training Unit. “They are informed by the experience of our country teams and partnerships, offering real-world solutions that have worked in a variety of settings and can be tailored to address specific challenges.”
The fourth and final resource, “Starting Antiretroviral Therapy in the Era of Treat All,” includes a variety of clinical and monitoring and evaluation resources. The document’s seven sections cover retesting for verification of HIV status, key counseling messages, rapid ART initiation, clinical follow-up, community ART initiation, monitoring and evaluation of programs, and key health systems considerations. Special considerations for initiating ART in infants, children, and adolescents are included, as well as care guidelines for patients with advanced disease.
“The science absolutely supports rapid ART initiation in people living with HIV, but a patient-centered approach is needed so people who are newly diagnosed don’t feel overwhelmed, but rather confident about their options and decisions in managing their health,” said Ruby Fayorsey, MD, MPH, deputy director in ICAP’s Clinical and Training Unit. “Our resource on ART initiation gives clinicians tools and key messaging points to talk with patients about their status, assess their readiness to begin ART, and work with them to start on these lifesaving medications.”
ICAP offers a range of toolkits to help clinicians, health care workers, and outreach specialists incorporate innovations and best practices into their work. Both the Viral Load Toolkit and Pre-exposure Prophylaxis (PrEP) Package have been translated into multiple languages. Additional tools and resources are available on the organization’s website.