In efforts to boost the resiliency of Sierra Leone’s health systems after a six-year period of natural disasters and public health emergencies, ICAP at Columbia University is spearheading a series of projects to strengthen the national health system’s practices in infection prevention and control, or IPC. This initiative aims to form a cadre of IPC specialists across the country, increasing health system resiliency and responsiveness through quality improvement and human resource development.
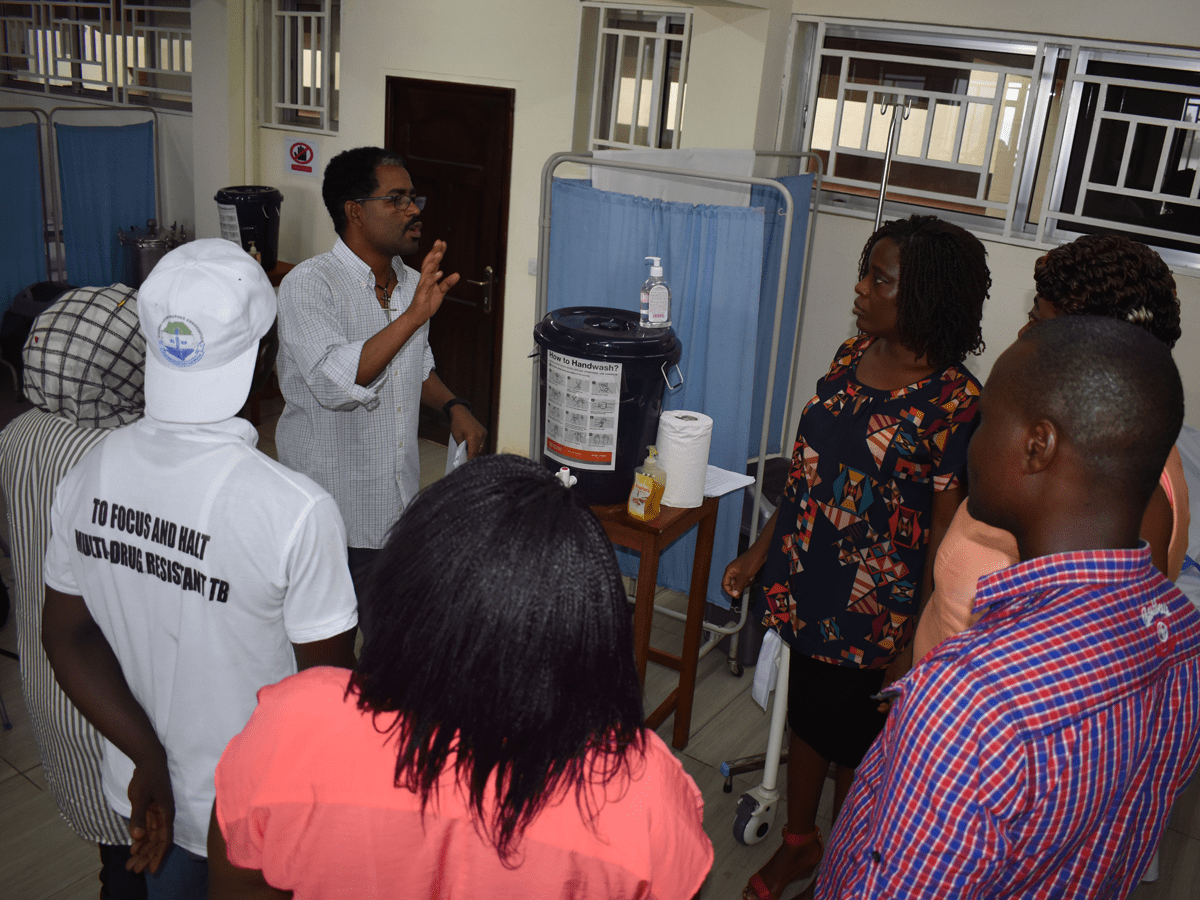
In 2014, Western Africa faced the largest health emergency in its history with the rapid community spread of Ebola, a deadly viral hemorrhagic fever that spreads through direct contract with the bodily fluids of a person who is sick with or has died from Ebola virus disease. During the epidemic, Sierra Leonean health workers were 21-32 times more likely to be infected with Ebola than the general population, and it is estimated that as much as one in five members of the health work force died from the highly contagious virus. A lack of critical knowledge of IPC—including use of personal protective equipment, handwashing, and cough hygiene practices—has been cited as a driving force for the rapid spread of Ebola among health workers.
Under the leadership of the Sierra Leonean government, efforts made in the post-emergency response have emphasized the importance of widespread IPC knowledge among health workers as the cornerstone of a strong and resilient public health system. Through the support of the U.S. Centers for Disease Control and Prevention (CDC) and in partnership with Ministry of Health and Sanitation (MoHS) and the World Health Organization (WHO), ICAP developed an advanced certification program in IPC for frontline health workers.
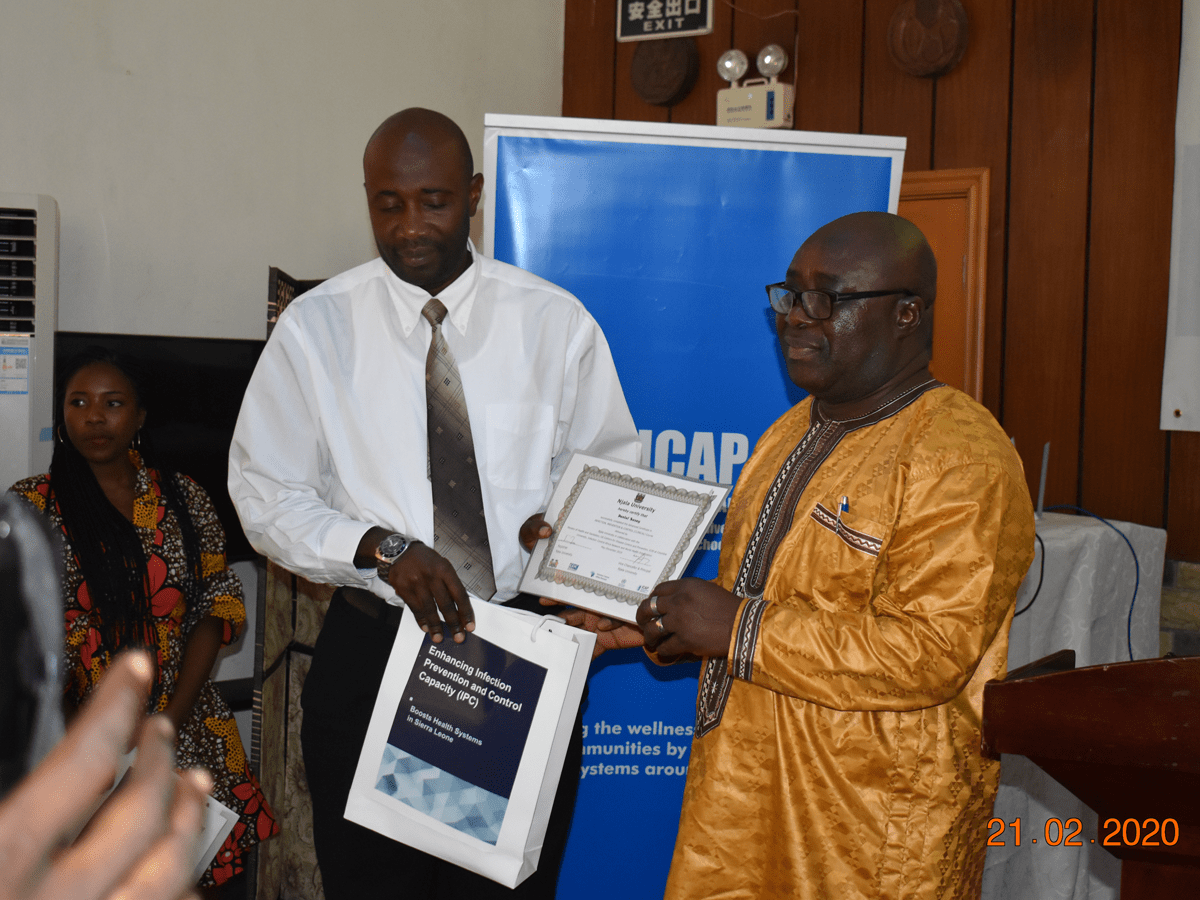
In February 2020, the first cadre of health workers completed the six-month program and marked the occasion at a graduation ceremony held in Freetown, Sierra Leone.
Dr. Thomas Samba, Chief Medical Officer, emphasized the importance of the project in his remarks saying, “The newly evolving landscape of infectious diseases across the world is a stronger justification for developing a pool of IPC experts in all countries, especially developing countries like Sierra Leone.”
Daniel Sesay, a graduate and health worker, shared his appreciation for the training: “We are grateful and indebted to ICAP, CDC, MoHS, for their continued support to improving the country’s health system. I believe we have [been] empowered to make a difference, and our [success] from the two weeks’ on-the-job training shows our preparedness and competence to support the development of this country’s health systems.”

The new graduates will disseminate their new expertise in IPC at each of their facilities. This infusion of knowledge and best practices to health facilities across the country comes at a critical time as Sierra Leone ramps up its response to the novel coronavirus.
A global health leader since 2003, ICAP was founded at Columbia University with one overarching goal: to improve the health of families and communities. Together with its partners—ministries of health, large multilaterals, health care providers, and patients—ICAP strives for a world where health is available to all. To date, ICAP has addressed major public health challenges and the needs of local health systems through 6,000 sites across more than 30 countries.