Dedicated and clinically competent nurses play a critical role in providing health care to people across the globe. Nurses are important health care providers in their own right, accounting for nearly half of the world’s health workforce globally. In ordinary times, nurses frequently serve as the primary touchpoint between patients and the health care system, providing clinical services, diagnostics, and testing. During health crises, nurses can hold the line against epidemics. A strong nursing force leads to improved health and wellbeing for patients and every initiative to strengthen a health system should take nurses into account. Inevitably, supporting nurses with training, equipment, and infrastructure translates into improved health outcomes.
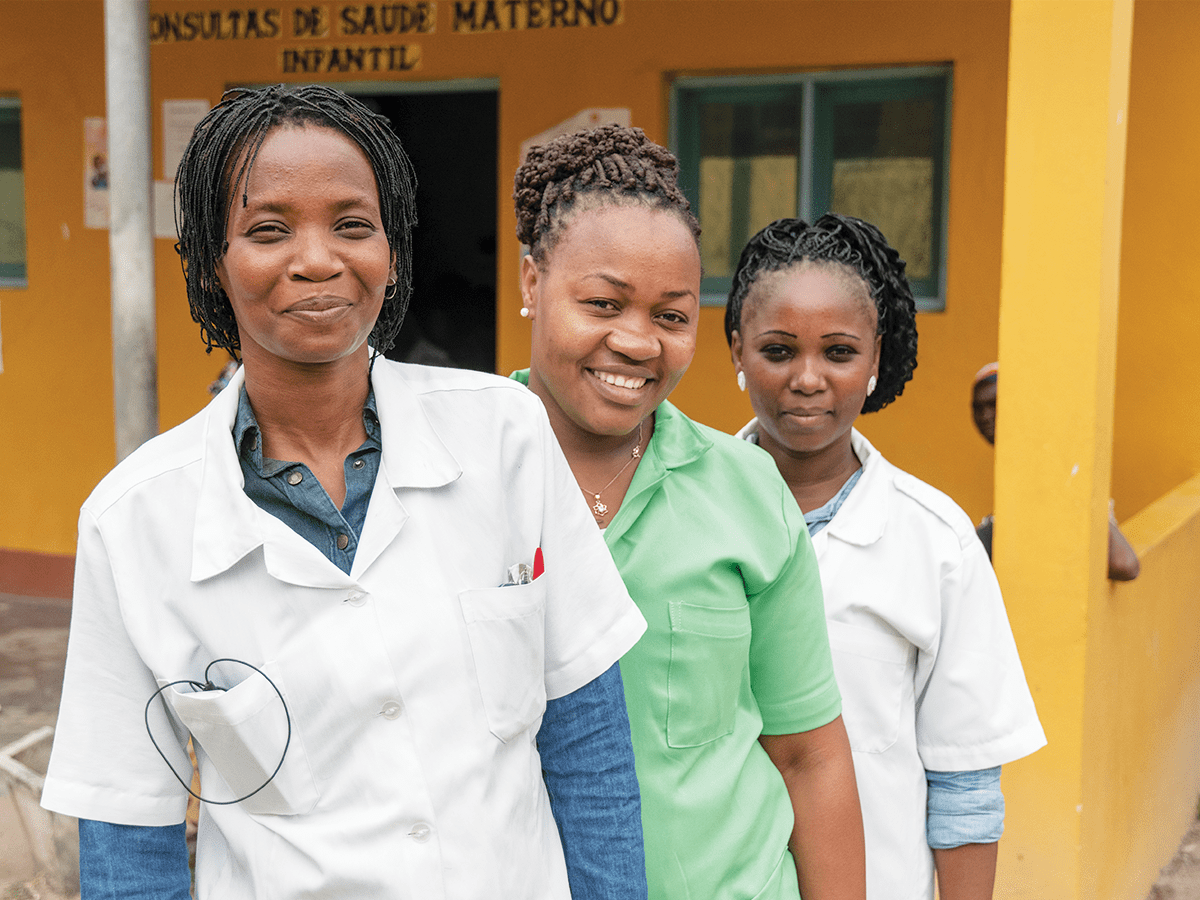
As the world commemorates the Year of the Nurse and the Midwife, ICAP honors the dedication of the nurses in its programs and in the everyday lives of patients around the world and emphasizes the outsized leadership role that they should play in delivering health care and shaping health policy.
On the Front Lines of Global Health
Although there is significant diversity in the responsibilities of nurses in different parts of the world, every nurse serves as an essential link between health systems and communities. Nurses can be found in schools, clinics, hospitals, airports, and at public events, serving as a first line of care ad bridge to the formal health system. They are therefore, often the first (and sometimes only) point of contact patients have with health systems. They are uniquely positioned to shape and deliver effective health interventions to meet the needs of patients in the communities they serve. In low-resource contexts, nurses form the frontline defense against the leading causes of mortality providing life-saving care for common illnesses such as malaria, pneumonia and tuberculosis. Nurses across Africa are often the only health workers available to patients and provide a wide range of health services, sometimes outside of their legal scope of practice because of extreme medical staff shortages and poor distribution of doctors in rural areas. Other nurses, especially those working in hospitals in low- and middle-income countries, are not used to their full potential and could be doing more to streamline initial intake procedures and routine screenings.
Despite their crucial role in health care, many countries face a shortage of nurses—a shortage further exacerbated by a lack of infrastructure to ensure ongoing training and education. Nurses with access to increased educational opportunities, such as Nurse Practitioners, can provide a wide array of services to their patients including diagnosis, prescriptions, and simple to complex procedures. In some countries and settings where nurses take on advanced scope of practice in such areas as obstetrics and anesthesiology, they provide life saving services where doctors are few and the burden of disease alarmingly high. This nurse-based approach greatly expands access to care, facility capacity and improves the quality of patient care. Whether a nurse is at the bed side, in a school or serving as a nurse specialist in cancer care or as a nurse anesthetist, they are often doing this where and when they are needed most. Provided care where few other providers can be found.
Not only has research shown that empowering nurses as leaders in health care and treatment leads to better patient outcomes, but global trends in health care continue to increase the scope of nurses. Changes in the burden of disease are having an outsize impact on health workers, as patients require care for more long-term conditions and non-communicable diseases (NCDs). Treatment for lifelong conditions associated with HIV and other conditions such as cardiovascular disease, diabetes, and cancer are increasingly needed and demand significant time and resources directed towards chronic care services. Nurses have become a dominant provider of non-communicable disease care as countries address the dual burden of infectious and non-infectious diseases. Nurses have therefore been increasingly critical to providing this community-based care, shouldering more and more responsibility as the workload for health systems increases.
Especially in low resource settings, patients with untreated chronic diseases will often only seek treatment when symptoms are present. In many instances, this is a point when treatment is more complicated and places a significantly greater strain on health systems and resources. Nurses, whose role places them at a critical junction between health systems and communities, are in a unique position to reverse the impact of NCDs by providing health promotion, early detection and treatment, illness prevention, treatment adherence, and rehabilitation in community settings.
“The wisdom and experience of nurses is fundamental to building health systems able to achieve universal health coverage rooted in strong models of primary health care,” said Susan Michaels-Strasser, PhD, MPH, RN, FAAN, senior implementation director and associate director for nursing programs for ICAP. “Globally, nurses are at the frontlines of primary health care; we can take the numerous lessons learned from HIV, where full engagement of nurses in comprehensive treatment programs has been a game changer around the world.”
Putting the Spotlight on Nurses
ICAP has over 17 years of experience providing impactful and sustainable technical assistance, capacity building, and implementation support to ministries of health and other stakeholders. ICAP’s team of global and local experts combine forces to deliver state-of-the-art approaches to tackling complex health service development, scale-up, and quality issues around the world. This capacity-building approach utilizes a participatory and iterative process to examine, design, implement, and monitor all project activities.
In countries where ICAP works, nurses provide up to 90% of care. But in these countries, training and retaining enough skilled nurses is a serious challenge for the public health systems. As its portfolio of technical assistance has expanded, ICAP has prioritized strengthening nursing and midwifery education, continuing professional development, and enhancing professional networks at all levels of public health systems in program countries.
Class Act
In Sierra Leone, ICAP has been working with the Sierra Leone Ministry of Health and Sanitation since 2017 to increase the number of trained midwives and decrease the country’s rates of maternal and infant mortality, which are among the highest in the world. These efforts are part of the Resilient and Responsive Health Systems Project, funded by the U.S. Health Resources & Services Administration (HRSA). To date, ICAP has supported all three schools of midwifery in Sierra Leone and their affiliated hospitals and the College of Medicine and Allied Health Sciences (CoMAHS) at the University of Sierra Leone.
ICAP has led a number of projects to strengthen curricula, improve training for instructors and mentors, and increase practical learning opportunities for students through simulation-based training and skills labs and clinical practice with trained preceptors. ICAP introduced curriculum modules on critical subjects such as HIV testing, care and treatment; infection prevention and control; and emergency obstetric care. At the same time, ICAP has improved training infrastructure for students and instructors through the provision of textbooks and computers for university libraries and the stocking of training labs with personal protective equipment and high fidelity simulation mannequins.
These efforts were part of the Resilient and Responsive Health Systems Project, funded by the U.S. Health Resources & Services Administration (HRSA).
A Personal Connection
Nurses also play a central role in community based ICAP programming for people living with HIV in Central Asia, where rising levels of dependency on injectable drugs is closely linked to the resurgence of HIV infections. Access to lifesaving HIV treatment once infected with the virus is challenging for people in highly stigmatized groups—including people who inject drugs, sex workers, and men who have sex with men—because of high levels of stigma, lack of family support, and costs related to health care (i.e. travel time and costs, clinic wait times, and income loss).
ICAP’s Support4Health project uses a home-based care model to train and mentor nurses from health facilities who then extend services into the community, targeting patients who are not able or willing to attend appointments at HIV care and treatment clinics. Dinara Salimbayeva, a nurse at the ICAP-supported East Kazakhstan AIDS Center regularly travels to patients’ homes to provide outreach, education, and adherence support. “Sometimes it takes a personal connection to help someone get to where they feel confident in their own ability to care for their health,” Salimbayeva said. The home visits, she went on to explain, help build a trusting relationship with a health professional and enable her to offer specific support for patients’ needs, without their having to risk identification and stigma by visiting a health facility. During home visits, nurses conduct monitoring of adherence to HIV treatments; remind patients about their scheduled clinical visits; provide information on nutrition, side effects, and HIV prevention methods; and refer patients to methadone therapy programs.
The program was supported by PEPFAR through the Centers for Disease Control and Prevention (CDC). The program, which began in 2015, is now being implemented at all 28 health facilities ICAP supports in Central Asia.
Strength Training
Nurses also play a central role in community based ICAP programming for people living with HIV in Central Asia, where rising levels of dependency on injectable drugs is closely linked to the resurgence of HIV infections. Access to lifesaving HIV treatment once infected with the virus is challenging for people in highly stigmatized groups—including people who inject drugs, sex workers, and men who have sex with men—because of high levels of stigma, lack of family support, and costs related to health care (i.e. travel time and costs, clinic wait times, and income loss).
ICAP’s Support4Health project uses a home-based care model to train and mentor nurses from health facilities who then extend services into the community, targeting patients who are not able or willing to attend appointments at HIV care and treatment clinics. Dinara Salimbayeva, a nurse at the ICAP-supported East Kazakhstan AIDS Center regularly travels to patients’ homes to provide outreach, education, and adherence support. “Sometimes it takes a personal connection to help someone get to where they feel confident in their own ability to care for their health,” Salimbayeva said. The home visits, she went on to explain, help build a trusting relationship with a health professional and enable her to offer specific support for patients’ needs, without their having to risk identification and stigma by visiting a health facility. During home visits, nurses conduct monitoring of adherence to HIV treatments; remind patients about their scheduled clinical visits; provide information on nutrition, side effects, and HIV prevention methods; and refer patients to methadone therapy programs.
The program was supported by PEPFAR through the Centers for Disease Control and Prevention (CDC). The program, which began in 2015, is now being implemented at all 28 health facilities ICAP supports in Central Asia.
Celebrating Nurses
“In my role as director for nursing programming at ICAP, I’ve been profoundly touched by the passionate dedication of nurses I have met around the world,” shared Dr. Michaels-Strasser. “This was especially clear to me in the midst of the Ebola outbreak in Sierra Leone in 2014 and 2015. We watched as nurses put their lives on the line to deliver care to communities at a time of immense fear and uncertainty. They became advocates for patients and their families, and additionally served as critical cross-cultural liaisons for international experts providing extra support during the crisis. But even in ordinary times, nurses are at the heart of health care and their deep knowledge of the communities that they serve is critical to the improvement of any health system. Our work at ICAP seeks to build up nurses as strong leaders and advocates for health around the world.”
This year, and every year, ICAP celebrates the contribution of nurses and midwives. For ICAP, nurses are at the heart of any solution for the world’s most pressing health challenges. With nurses at the helm advocating for patient-centered approaches in health care and health policy, practical and affordable solutions for the world’s most pressing health challenges are reachable.
This article is part of ICAP’s 2020 Year of the Nurse campaign to advocate for nurses as leaders in the international health sector and encourage discussion on how the global health world can better leverage nurses’ unique connections to the communities they serve.
With nurses at the helm advocating for patient-centered approaches in health care and health policy, practical and affordable solutions for the world’s most pressing health challenges are reachable.
Learn more about our work with, and for, nurses on our campaign page, #ThisNurseCan.
—
A global health leader since 2003, ICAP was founded at Columbia University with one overarching goal: to improve the health of families and communities. Together with its partners—ministries of health, large multilaterals, health care providers, and patients—ICAP strives for a world where health is available to all. To date, ICAP has addressed major public health challenges and the needs of local health systems through 6,000 sites across more than 30 countries.