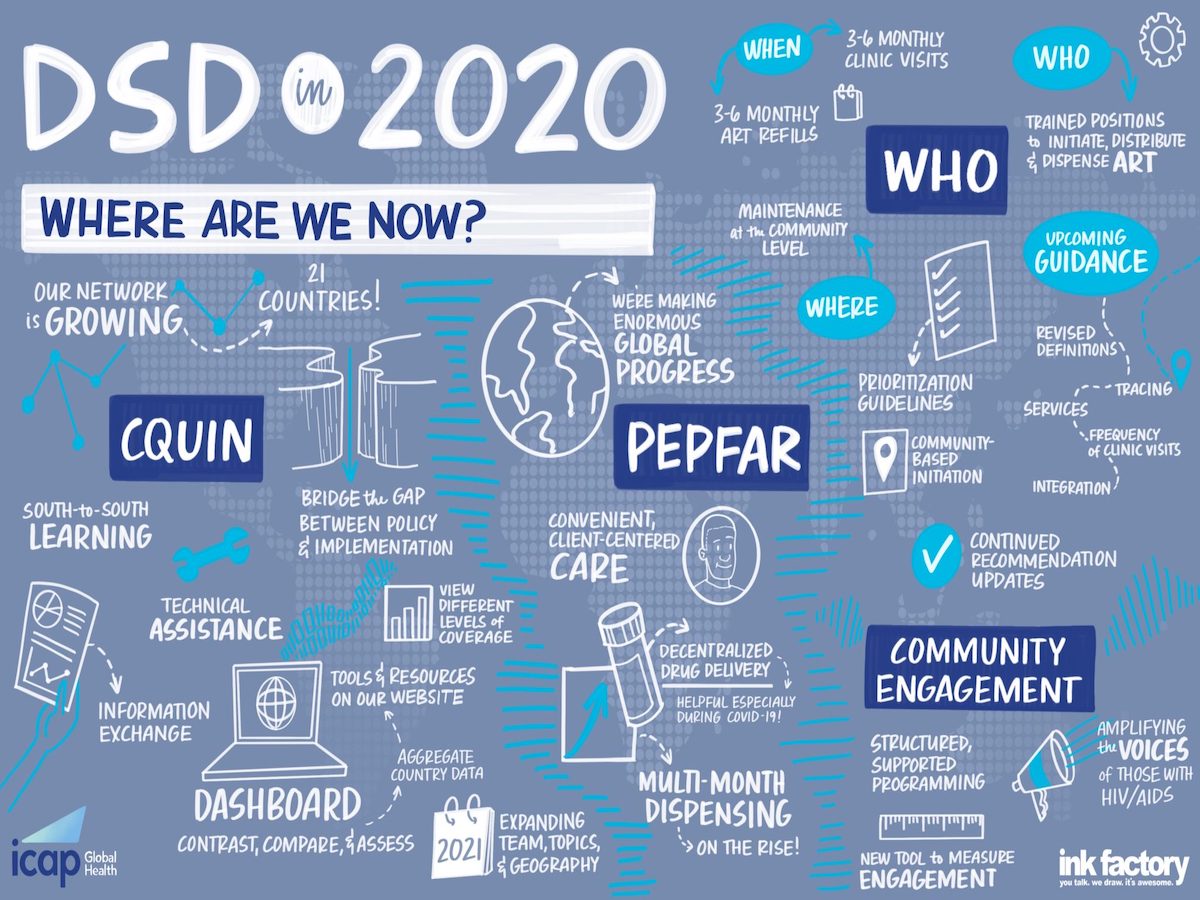
Since 2018, ICAP’s HIV Coverage, Quality, and Impact Network (CQUIN) has convened network member countries and their ministry of health representatives, national networks of people living with HIV, communities, global partners such as the President’s Emergency Plan for AIDS Relief (PEPFAR), the World Health Organization (WHO), the Global Fund, the International Aids Society (IAS), the International Treatment Preparedness Coalition (ITPC), and others for the CQUIN annual meeting.
The annual meeting is the network’s showcase event, giving CQUIN member countries an opportunity to review and present data on the progress made toward implementing and scaling up differentiated service delivery (DSD) and gaining epidemic control over the past year. At this year’s meeting, CQUIN countries also reviewed DSD adaptations they made toward the COVID-19 pandemic.
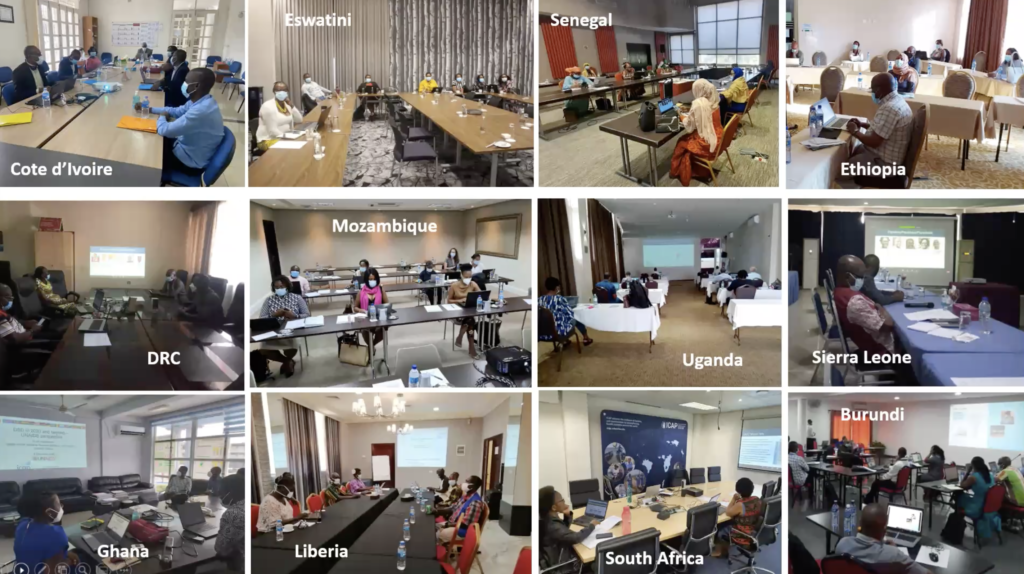
The annual meeting, usually held in one of the now 21 CQUIN member countries, was held virtually this year from December 7-10, 2020, due to the COVID-19 pandemic, bringing together over 450 participants.
“The COVID-19 pandemic had a dramatic impact on HIV programs worldwide. CQUIN’s major activities such as the community of practice meetings and south-to-south learning exchanges have not been exempted,” said Miriam Rabkin, MD, MPH, ICAP director for Health Systems Strategies and principal investigator for CQUIN. “In response, CQUIN has pushed all major activities online by facilitating more virtual exchange of information, tools, and resources related to the adaptation of DSD policy and implementation in response to COVID-19, helping network countries maintain the resilience of their national HIV treatment programs during the pandemic.”
With 12 sessions, including plenary presentations, panel discussions, parallel sessions, and breakout group discussions, the four-day virtual conference focused on the challenges and successes made toward improving health care outcomes for people living with HIV. Here is a round-up of key takeaways from the annual meeting.
Bridging the Gap Between HIV Policy and Program Implementation
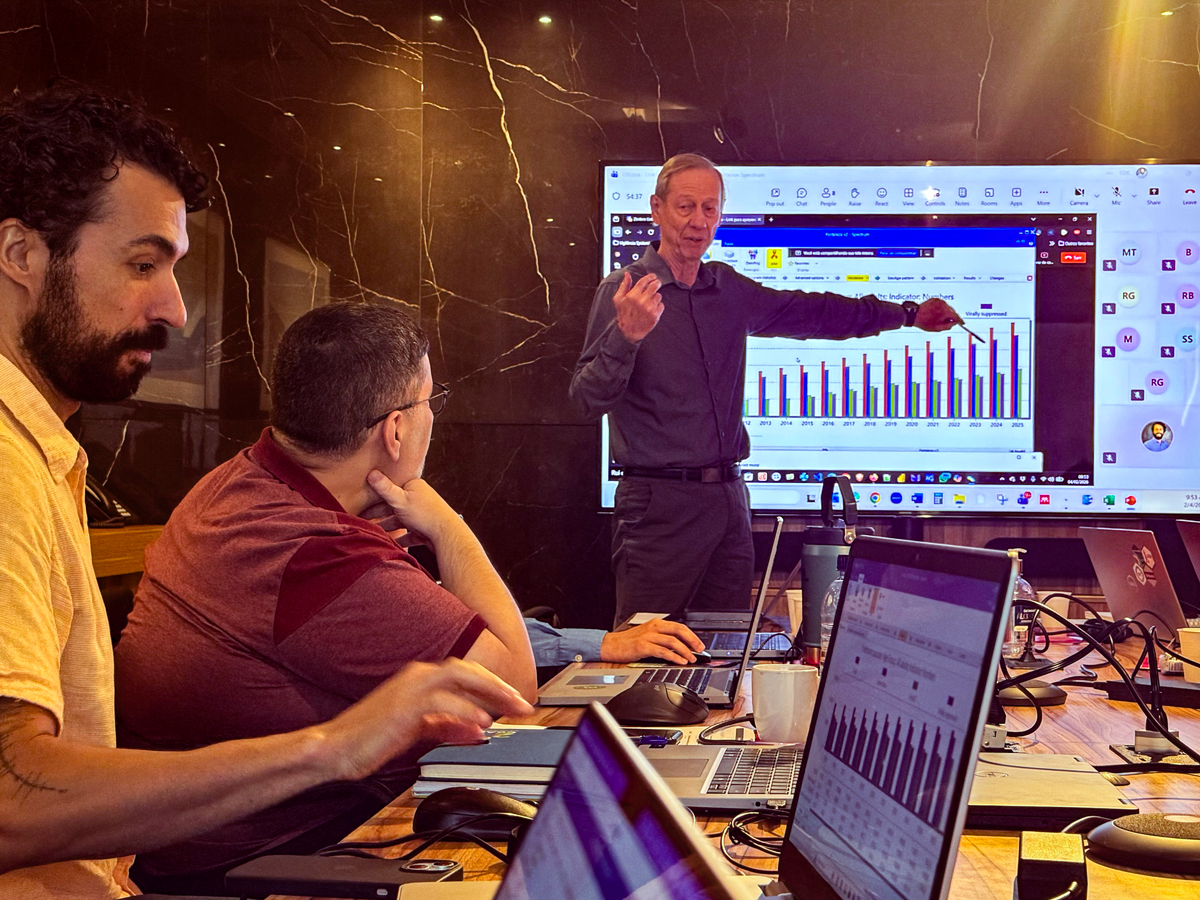
Continuing to find innovative and convenient ways of encouraging optimal service delivery for recipients of care was the annual meeting’s running theme. Seven plenary presentations by various CQUIN stakeholders and partners provided an overview of the current state of HIV care and DSD.
Dr. Rabkin provided a snapshot of the CQUIN network’s growth from six countries to 21 countries in four years. She also talked about the communities of practice (time-limited initiatives and groups focused on developing specific resources and tools for these groups, such as the Advanced HIV Disease and Monitoring and Evaluation communities of practice) initiated over the past year. Most importantly, Dr. Rabkin gave an overview of the CQUIN DSD dashboard – the network developed self-assessment tool and data used to help countries measure the progress of DSD programs to ensure coverage of quality HIV care services as the number of differentiated antiretroviral therapy (DART) models. “Understanding the range and distribution of the models and how they change over time can be tremendously helpful to ministries of health and their partners as they plan their national HIV strategies for the coming year,” Rabkin said in her presentation.
In the same session, Catherine Godfrey, MD, senior technical advisor for Adult Care and Treatment, Office of the Global AIDS Coordinator, gave a comprehensive update on PEPFAR policy adaptations this year, such as therapeutic alliance (the right care, at the right time by the right provider) with a focus on treatment continuity and overcoming the barriers to HIV treatment. “DSD models are a response to the barriers that threaten the alliance of care, and PEPFAR aims to address the diverse needs of all recipients of care,” Godfrey said.
Nathan Ford, MD, a scientific officer with the Department of HIV, Viral Hepatitis, and STIs, WHO, gave an overview of some recommendations and updated guidelines countries can look forward to from the international organization, including a revised definition of people who are stable on ART, and recommendations on giving ART outside of the health facility setting.
Bactrin Killingo, MD, treatment, and education lead, ITPC, gave the perspective from the community of people living with HIV. He reiterated the importance of community engagement at the policy level in implementing HIV programs. “This year, we have been able to provide guidance on what community engagement is and have come up with a tool that can measure community engagement and score whether or not people are meaningfully engaged to pilot in two countries in the first quarter of next year,” Dr. Killingo said. The Global Fund, UNAIDS, and IAS also made presentations.
The Impact of COVID on Differentiated Service Delivery
Wafaa El-Sadr, MD, MPH, MPA, ICAP’s global director, presented a snapshot on the effects of COVID-19 on HIV programs and health services in Africa and lessons learned from the COVID-19 emergency response so far. “COVID-19 has impacted health systems in terms of decreased supply or decreased demand. The cancellation of elective surgeries, outpatient visits, the diversion of resources to the COVID-19 emergency response, people avoiding health care facilities for fear of infection, lockdown restrictions, staff reassignments, and economic hardship that makes it difficult for people to access health services,” said El-Sadr.
However, El-Sadr also highlighted the innovations and progress some ICAP member countries, including South Sudan, Tanzania, DRC, and Mozambique, have made to DSD in response to COVID. “COVID-19 has motivated rapid change in program design in response to the urgency of the pandemic, and this perhaps this is the silver lining from this pandemic,” she said.
El-Sadr’s presentation was followed by a panel discussion on country adaptations to COVID, with specific examples from Uganda, Zimbabwe, and Rwanda from policymakers and recipient- of-care communities.
Parallel Sessions: Country DSD Updates and Breakout Sessions
In nine parallel country sessions, 19 countries gave brief overviews of their country context, strengths, programs, and models implemented in the country to advance HIV service delivery. Panel discussions among ministry of health representatives, recipients of care, and other program implementing partners followed the country presentations. The panel discussions encouraged interaction and fostered learning through question-and-answer sessions between presenters and participants on country progress towards DSD.
Breakout Sessions: Focus Areas
Meeting participants could also choose between nine parallel breakout sessions on various focus area topics throughout the four-day meeting. The focus area topics were Viral Load Access, DSD for Mobile and Displaced Populations, Community Based DSD Models, DSD for People with HIV and Non-Communicable Diseases (NCDs), Differentiated Maternal and Child Health Services, Accessing HIV Services During COVID-19, Differentiated HIV for Key Populations, and DSD for Advanced HIV Disease. Each session included at least five presentations using country, context-specific experiences, and case studies to paint a picture of the situation on the ground. All presentations encouraged engaging discussions and question and answer sessions between panelists and participants.
DSD is More than Multi-Month Dispensing: Looking Ahead to 2021
Expanding the topics of discussion, coverage quality within West and Central Africa with the development of a new regional hub, and a resumption of in-person meetings and activities such as the south-to-south country learning exchanges are a few activities members of CQUIN can look forward to in 2021.
Peter Ehrenkranz, MD, MPH, senior program officer, HIV Treatment with the Bill and Melinda Gates Foundation, which funds CQUIN, in his closing remarks, encouraged network country representatives to continue thinking of how to implement sustainable HIV services for the people who need them the most. “Multi-month description is a really important tool for delivering people-centered care, but it is not the only one. Retention and viral load suppression are important but not sufficient in determining that we are delivering people-centered care that can be sustained over time,” Ehrenkranz said. He charged ministries of health to include regular patient assessments of provider services in developing their annual targets and work plans.
Burundi, Côte d’Ivoire, DRC, Ghana, Kenya, Uganda, South Africa, and Zimbabwe held separate in-person breakout sessions to develop their CQUIN DSD work plans to expand HIV care implementation targets for 2021.
Côte d’Ivoire plans to employ a national DSD coordinator whose sole attention will be to increase coverage and services for diverse patients. Uganda intends to emphasize more involvement from the recipients of care in planning and determining the satisfaction of HIV services.
To access all the annual meeting resources, visit the CQUIN website.
Learn more about CQUIN, and what the network has achieved in the last four years in the video below.