Researching Biomedical Responses to COVID-19

Recognizing the urgency of developing prevention and treatment responses to COVID-19, ICAP rapidly mobilized efforts at its two longstanding research sites in New York City, the Bronx Prevention Center and Harlem Prevention Center. Their decades of experience in conducting research in their resource-challenged New York City communities have positioned these centers to ensure their clinical trials include the diverse study populations critical for mounting a robust and equitable public health response.
At the Harlem Prevention Center, ICAP participated in the ENSEMBLE study, involving over 50,000 volunteers over age 18, with significant representation of people over the age of 60, testing a single-dose vaccine by Janssen, a division of Johnson & Johnson, which would eventually become the third vaccine approved for emergency use in the US.
In the adjacent community of the Bronx, ICAP participated in a Phase III trial to assess the safety, efficacy, and immunogenicity of the Oxford-AstraZeneca vaccine, which would go on to be put into use in countries around the world.
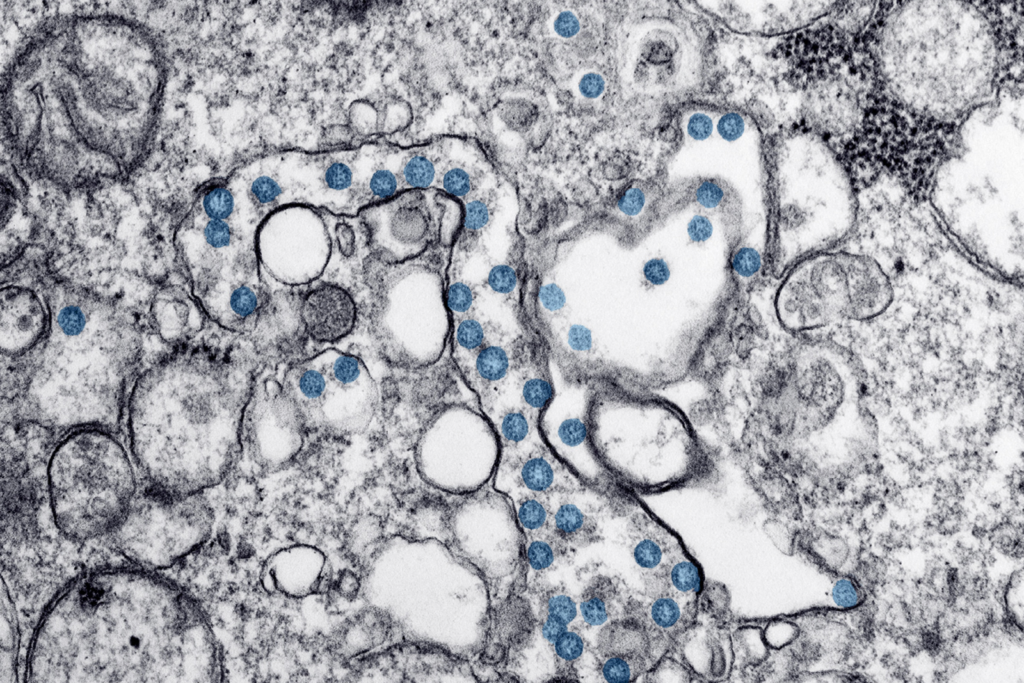
Both centers have also participated in the Community Prevalence of SARS-CoV-2 Study – also known as COMPASS – a nationwide initiative led by the National Institute of Allergy and Infectious Diseases, involving approximately 16 communities across the United States.
Among the questions the study is investigating are the role of children in community transmission, what demographic and social risk factors contribute to infection rates, and which medical co-morbidities are associated with seroprevalence. The study is also investigating important factors that can affect the spread of the virus including racial and ethnic disparities in access to testing and health resources, and community attitudes around efforts to contain transmission.
“The data collected through this population-based survey will give us a greater understanding of the extent of current and prior COVID-19 and will therefore help us project future disease risk,”
Jessica Justman, MD,
ICAP’s senior technical director
and principal investigator of the study for ICAP
Against the backdrop of the pandemic, ICAP has also undertaken two studies to assess the burden of COVID-19 on key vulnerable populations in New York City:
The Silver Study set out to garner a deeper understanding of the physical, emotional and economic impacts of COVID-19 on elderly populations most impacted by COVID-19 in NYC by conducting surveillance of their present experiences and insights during the pandemic with the goal of shaping an effective response to their needs.
The LEXICON (LGBTQ+ Experience In COVID-19 NYC Study) is designed to explore the toll of COVID-19 on the LGBTQ+ population in New York City, through a survey to measure uptake of testing, interventions such as social distancing and masking, and vaccination, with additional questions to measure knowledge, attitudes, prevalence, and the burden of COVID-19 symptoms.
Both of these novel surveys seek to provide much-needed, actionable data to support New York City’s ability to respond to the needs of these communities.
Funding for research at the Harlem Prevention Center includes: National Institutes of Health/National Institute of Allergy and Infectious Diseases (NIH/NIAID), Department of Health and Human Services (DHHS), Family Health International (FHI), Janssen, Fred Hutchinson Cancer Research Center
Funding for research at the Bronx Prevention Center includes: National Institutes of Health/ National Institute of Allergy and Infectious Diseases (NIH/NIAID), Department of Health and Human Services (DHHS), Family Health International (FHI), AstraZeneca, Merck, Evofem, Gilead Biosciences, Fred Hutchinson Cancer Research Center
Funding for the Silver Study: New York Community Trust and the Samuels Foundation
Funding for the LEXICON Study: The Rockefeller Foundation
SCIENCE-DRIVEN
COMMUNITY-BASED
EQUITABLE

Advocating for Vaccine Equity
 An advocate for global health equity for decades, ICAP Global Director Wafaa El-Sadr joined two colleagues to write a New York Times Op-Ed to point out that unless vaccines with high efficacy can be quickly manufactured and made available broadly, we are at risk of failing to control the COVID-19 pandemic.
An advocate for global health equity for decades, ICAP Global Director Wafaa El-Sadr joined two colleagues to write a New York Times Op-Ed to point out that unless vaccines with high efficacy can be quickly manufactured and made available broadly, we are at risk of failing to control the COVID-19 pandemic.
“Viruses know no borders. Protecting Americans from COVID-19 requires protecting all people from COVID-19. We cannot end the COVID-19 pandemic until everyone, across the world, can access highly effective vaccines.”
Wafaa El-Sadr, MD, MPH, MPA, founder and director of ICAP,
The New York Times, Jan. 12, 2021
El-Sadr calls for aggressive government action in the United States to increase manufacturing capacity of the high-quality vaccines that are already proven and to provide support for global distribution. Reminding government leaders of the success of PEPFAR, created by President George W. Bush with guidance from NIAID director Anthony Fauci, which is estimated to have saved 19 million lives, El-Sadr and her colleagues suggest that the Biden Administration should once again demonstrate what can be accomplished with generosity and partnership.

Continuing HIV Research Undeterred
 While engaging with urgent research to tackle COVID-19, ICAP’s Harlem Prevention Center (HPC) and Bronx Prevention Center (BPC) have continued their vital research to prevent HIV infection and work they are doing under the auspices of the HIV Prevention Trials Network (HPTN) – a worldwide collaborative for clinical trials that brings together investigators, ethicists, community members and other partners to develop and test the safety and efficacy of HIV interventions. Because of deep roots in the Bronx and Harlem communities, which have been among the hardest hit by the HIV epidemic in the United States, HPC and BPC’s participation in the trials helps to ensure that key populations that are part of these local communities are represented in global research efforts.
While engaging with urgent research to tackle COVID-19, ICAP’s Harlem Prevention Center (HPC) and Bronx Prevention Center (BPC) have continued their vital research to prevent HIV infection and work they are doing under the auspices of the HIV Prevention Trials Network (HPTN) – a worldwide collaborative for clinical trials that brings together investigators, ethicists, community members and other partners to develop and test the safety and efficacy of HIV interventions. Because of deep roots in the Bronx and Harlem communities, which have been among the hardest hit by the HIV epidemic in the United States, HPC and BPC’s participation in the trials helps to ensure that key populations that are part of these local communities are represented in global research efforts.
Rates of infection have been dropping worldwide, and these hopeful studies are designed to identify additional science-based strategies that can help to halt further transmission in marginalized populations both through new approaches to pre-exposure prophylaxis (PrEP) as well as by creating a vaccine. HPTN 083, a PrEP study concluded in spring 2020 concluded that an injectable form of PrEP is far superior to daily oral medication in lowering HIV incidence among both cisgender men and transgender women who have sex with men. Another PrEP study, HPTN 091 – also known as the I AM study – is assessing how to increase PrEP uptake among transgender women by combing PrEP with essential support services such as providing gender-affirming hormone therapy and peer health navigation.
The need for a safe and effective vaccine to prevent HIV remains urgent. In traditional vaccine studies, people are inoculated and then followed to see if their bodies will respond by making antibodies against HIV. A new idea for HIV prevention is to inject antibodies into people directly, rather than using a vaccine to trigger antibody production. ICAP has been part of the clinical trials for this new approach. Initial results from the Antibody Mediated Prevention Study (HPTN 085) demonstrated efficacy in protecting against certain strains of HIV). Researchers at HPC are also part of the ambitious Mosaico study, which is testing an investigational vaccine regime to prevent HIV. Also known at HVTN 706, this study is testing the efficacy of vaccines that are made from synthetic copies of HIV pieces – created in the laboratory – that cannot themselves cause HIV infection or AIDS. The study will enroll cisgender men and transgender people who have sex with cisgender men and/or transgender people.
More Impact Stories
Story One
Pivoting to Protect Vulnerable Populations
Story Two
Training Frontline Health Care Workers
As the COVID-19 pandemic arrived in Sierra Leone, ICAP's experience in health care worker training, mentoring and supportive supervision proved to be a critical asset.
Story Three
Researching Biomedical Responses to COVID-19
Recognizing the urgency of developing prevention and treatment responses to COVID-19.
Story Four
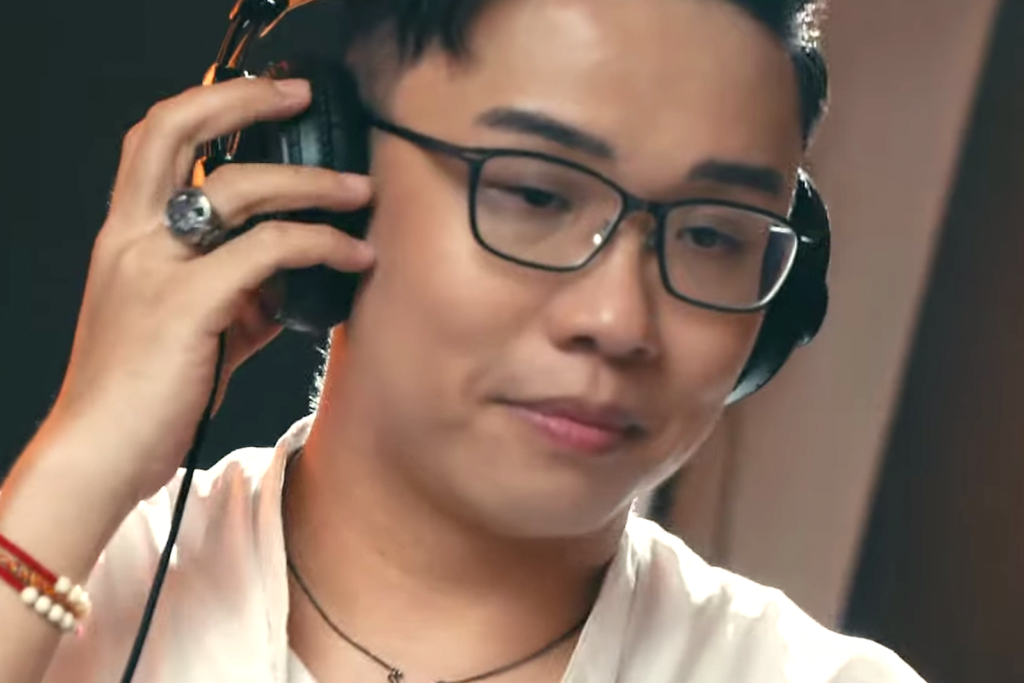
Saving Lives with Music
Story Five
Sustaining Methadone Treatment During Lockdown
Story Six
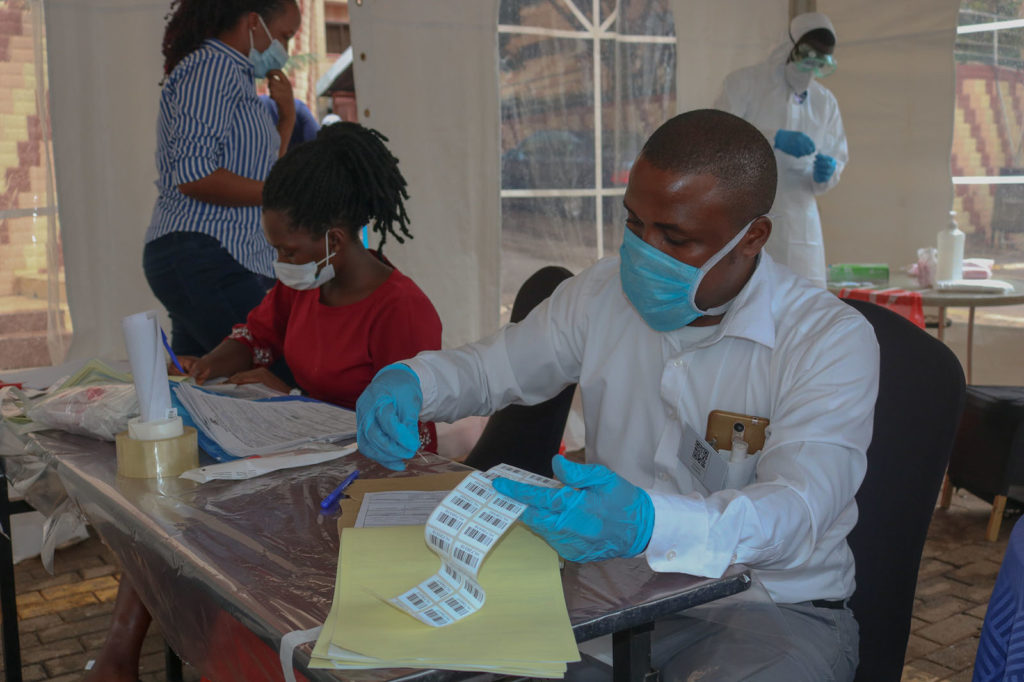
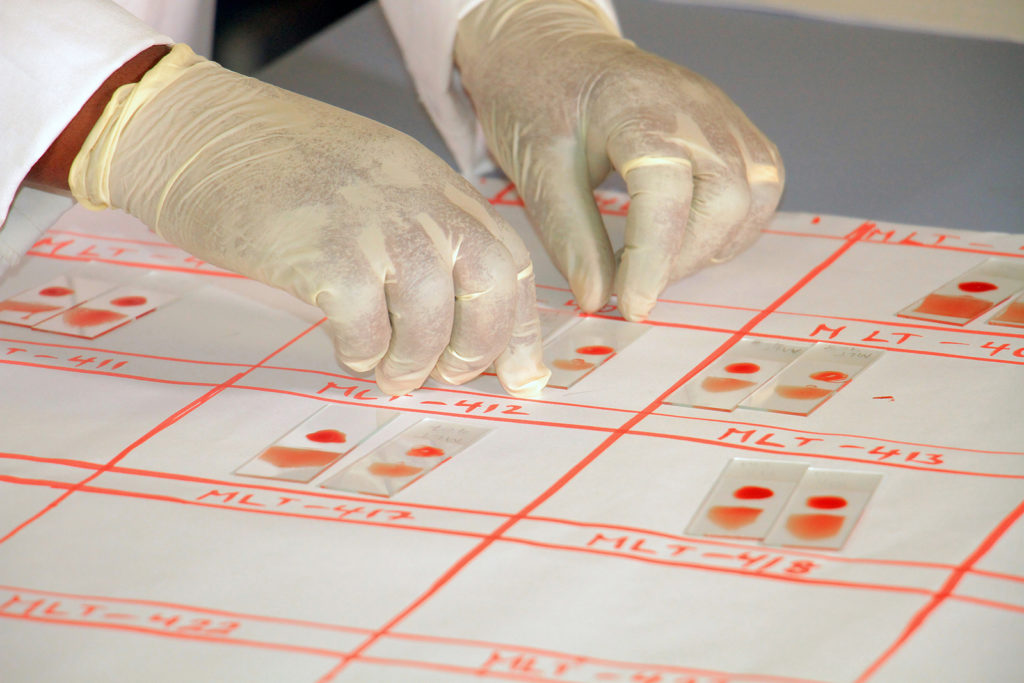
Harnessing Tech to Advance HIV Recency Testing
In the early days of the COVID pandemic, Zimbabwe had low infection rates, and people knew very little about the rapid global spread of the virus.
Story Seven
Surveying the HIV Epidemic Undaunted
Since 2014, the Population-based HIV Impact Assessment (PHIA) Project has been guiding the global HIV response by conducting national representative surveys that chart the state of the HIV epidemic across 15 countries.
Story Eight
Responding to Malaria in Remote Regions
For people who suffer from stigma and fear, including sex workers...
Story Nine
Confronting the Threat of Antimicrobial Resistance
While the rapid spread of COVID-19 continues to dominate headlines around the world, another health crisis looms large.
Story Ten
Connecting Key Populations to Care
For people who suffer from stigma and fear, including sex workers.