
2021 ICAP Impact Report
Going the Distance for Global Health
Read Report
Letter from the Director
ICAP’s founder and global director, Wafaa El-Sadr, MD, MPH, MPA, reflects on a year dedicated to moving forward—revisiting the daunting challenges of a global pandemic and reflecting on the power of ICAP’s unique model to meet everyday health emergencies effectively, efficiently, and equitably.

Where We Work
ICAP has worked in nearly 50 countries
Our IMPACT
In 2021, ICAP led numerous health initiatives in countries around the world in support of our mission to transform the health of populations through innovation, research, and global collaboration. The stories that follow provide a glimpse into how ICAP went the distance to support public health in communities worldwide.

Service
Research

Training & Education

Impact Measurement
SERVICE
Expanding access, improving health
ICAP supports evidence-based solutions aimed at addressing some of the world’s most challenging health issues, including HIV/AIDS, COVID-19, tuberculosis, malaria, emerging infections, non-communicable diseases, maternal and child health, and more. Through strategic partnerships and innovative projects, ICAP works alongside a diverse range of stakeholders to strengthen health systems and improve health outcomes in communities, countries, and regions around the world.
*Oct 2020-Sept 2021
**COVID-19 tests administered in Lesotho and Democratic Republic of Congo
*** Individuals vaccinated against COVID-19 in Sierra Leone and Tanzania
Featured Service Story
An Innovative Approach Brings HIV Care to Youth in Burundi and Nigeria

As governments worldwide responded to COVID-19 by mandating quarantines, health facility and school closures, and more, maintaining lifesaving HIV services became more critical – and challenging – than ever, particularly for young people living with HIV.
Globally, 54 percent of children living with HIV have access to treatment. In Burundi and Nigeria, only 31 and 45 percent of children living with HIV, respectively, were receiving treatment in 2020. The problem ICAP needed to solve was how to improve those numbers and get more young people living with HIV the care and treatment they needed amid the pandemic’s restrictions.
One part of the puzzle was solved by multi-month dispensing. This innovative approach works to provide patients with three to six months of medication at a time. While multi-month dispensing for adults living with HIV quickly became standard practice during the pandemic, many providers were reluctant or unable to fully adopt the approach for younger patients. Numerous factors contributed to this reluctance including nationally mandated age restrictions for multi-month dispensing, shortages of pediatric antiretroviral drug formulations, and provider perceptions that multi-month dispensing was not practical for growing children who required regular dosage adjustments.
Under the Reaching Impact, Saturation, and Epidemic Control (RISE) initiative, ICAP in Burundi and Nigeria worked to overcome these obstacles and increased enrollment of the number of children and adolescents living with HIV in community-based programs. Widespread adoption of multi-month dispensing, including for younger patients, helped reduce monthly medication refill visits, ultimately minimizing congestion and potential exposure to the coronavirus at health facilities.
ICAP in Burundi and Nigeria not only ensured young people were on optimized treatment regimens, but also partnered with community-based organizations to deliver medication refills and provide holistic services to young people and their caregivers at home.
“By bringing together individuals working in different areas of the HIV response, ICAP was able to foster collaboration from a wide variety of stakeholders to improve overall HIV care, including the provision of multi-month dispensing, for young people on treatment,” said Nandita Sugandhi, associate research scientist and pediatrician at ICAP.
Funder: U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) and the U.S. Agency for International Development (USAID)
Project: Reaching Impact, Saturation, and Epidemic Control (RISE) in collaboration with Jhpiego
More Stories
By Land and Water, FIKIA Reaches Key Populations with HIV Services in Tanzania

Taming the HIV epidemic requires going beyond the walls of hospitals and clinics. It calls for reaching out to people where they live, work, and socialize.
For the past five years, through a project known as FIKIA (“to reach” in the Kiswahili language), ICAP has brought critical HIV health services directly to communities in Tanzania, via motorcycle, mobile clinic, car, and boat. These HIV health services connected with populations at risk for HIV – sex workers, people who inject drugs, men who have sex with men (MSM), adolescent girls and young women, migrant workers, fisherfolk, and miners.
Since FIKIA’s inception, the project has reached more than two million individuals with HIV prevention, testing, treatment, and counseling services through innovations like backpack testing, which, as the name implies, lets health care workers bring testing to people at risk of HIV wherever they are in the community.
Building on the successes and lessons learned of this landmark outreach program, ICAP has embarked on a new project – called FIKIA Plus – which aims to support health facility and community-based HIV services that are tailored to the needs and preferences of communities in Mwanza, one of the largest regions in Tanzania and a key priority area for reaching epidemic control in the country.
Funder: President’s Emergency Plan for AIDS Relief (PEPFAR) through the U.S. Centers for Disease Control and Prevention (CDC)
Project: Comprehensive Community-Based HIV Prevention, Linkage, and Retention Services for Key Populations and Adolescent Girls and Young Women in the United Republic of Tanzania
Mobile TB and HIV Services Drive Health Forward in Mozambique

To be effective, critical health services must reach people who need them, which often means bringing services to where they are. In Mozambique, ICAP supported the delivery of comprehensive HIV and tuberculosis (TB) prevention, care, and treatment services – on wheels.
Mobile clinics and mobile brigades in 18 districts of Nampula province served 14 key population hotspots, 13 prisons, and six private companies. Using mobile health units, the teams provided all sites with HIV and TB services, including HIV and TB testing, treatment initiation, and psychosocial support, integrated with general health services, such as outpatient consultation, immunizations, and family planning.
Systematic screening in waiting areas helped fast-track individuals for the services they needed, whether that be early infant diagnosis for HIV-exposed infants, TB diagnostic testing for presumptive TB, or connecting eligible patients to TB preventive treatment (TPT). All TB presumptive cases and those eligible for TPT were entered into a register, receiving phone reminders for appointments until treatment completion.
From October 2021 to March 2022, of the 11,396 people living with HIV who visited an ICAP mobile clinic or brigade in Mozambique, 11,185 were screened for TB and 26 screened positive. Thanks to this program, 3,093 of the 3,795 individuals who initiated TPT through the mobile clinics and brigades completed the TPT cycle.
Funder: U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC)
Project: Advancing Sustainable Implementation of Comprehensive HIV/TB Services for Epidemic Control in the Republic of Mozambique
In the Kyrgyz Republic, Lab Training Boosts COVID-19 Response

Since the start of the COVID-19 pandemic, the Kyrgyz Republic in Central Asia wrestled with how to respond effectively to the crisis given the shortage of trained laboratory personnel able to perform diagnostic testing for the virus. Laboratories, especially in the capital city of Bishkek, were overwhelmed by the large number of samples that needed to be tested. Meanwhile, in other parts of the country – such as Naryn and Osh – staff who could perform PCR testing for COVID-19 were in very limited numbers.
In response, ICAP conducted practical skills-building workshops on PCR testing throughout the country, covering topics such as collection, storage, and transportation of samples; biosafety and biosecurity in the laboratories; and real-time PCR testing and interpretation of results. Following the workshops and two weeks of supervised practice, newly trained laboratorians were able to perform real-time PCR testing independently, giving the Kyrgyz people a critical tool for responding to COVID-19.
“Now I am doing PCR tests on my own. I am proud of myself. I feel my contribution in trying to combat COVID-19.” Zhusubakunova Tolkun Abykeevna, a laboratorian at the Naryn Center for Disease Prevention and State Epidemiological Surveillance
Funder: Centers for Disease Control and Prevention (CDC) and the CDC International Task Force (ITF)
Project: TRACE COVID ITF – CAR Lab/Diagnostics
ICAP’s Cervical Cancer Programs Save Lives Across Africa

In sub-Saharan Africa, cervical cancer is the leading cause of cancer deaths among women. Since 2009, ICAP has supported the screening and treatment of cervical cancer throughout the region, launching cervical cancer screening programs in Kenya, Mozambique, Eswatini, and Tanzania, and providing a range of support such as training nurses to provide cervical cancer screening and treatment, increasing linkages between HIV and women’s health care services, and disseminating clinical tools and materials to increase awareness about cervical cancer.
In many countries, the connection between HIV and cervical cancer is especially stark. Women living with HIV in Ethiopia, for example, are four to five times more likely to develop cervical cancer than those without HIV infection. To raise awareness about cervical cancer and reach more women who need access to screening and treatment in Ethiopia, ICAP supported the Ministry of Health to bring low-cost, safe, and effective cervical cancer services to 505 health facilities across six regions of the country.
At Dessie General Specialized Hospital – a major referral hospital in the Amhara region with high volumes of cervical cancer cases – ICAP helped establish a designated space for cervical cancer services within the HIV services clinic, providing necessary screening equipment such as speculums, and training health workers and support staff on how to use them. Following an ICAP-led analysis of electronic medical records to identify eligible patients, hospital health workers contacted more than 3,000 women eligible for screening and treated all 137 women who screened positive for precancerous lesions with cryotherapy or hysterectomies.
“The screening and treatment of precancerous lesions is simple and can be performed in a matter of minutes; however, the outcome is lifelong and lifesaving,” said Dr. Hezkiel Petros, cervical cancer program manager at ICAP in Ethiopia.
Funder: U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC)
Project: Technical Assistance to Ethiopia’s Federal Ministry of Health and Regional Health Bureaus in Comprehensive HIV/AIDS Programming and Direct Site-Level Support in the Four Emerging Regions under PEPFAR
With the Power of PrEP, ICAP Brings HIV Prevention to People Around the World

“I got a sense of safety and security thanks to PrEP,” said Adeline, a community member in Almaty, Kazakhstan, where ICAP recently supported the introduction of pre-exposure prophylaxis (PrEP). PrEP is a medication for people at risk of HIV. When taken daily, it can reduce the risk of HIV infection from sex by 99 percent.
Since 2017, ICAP has supported the implementation of PrEP through innovative person-centered programming that ensures individuals at risk of contracting HIV can access quality prevention services. Through ICAP’s projects, nearly 100,000 people across 15 countries have been initiated on PrEP, a key intervention to reduce new HIV infections and a critical component of epidemic control efforts. Following ongoing efforts in Burundi, Côte d’Ivoire, Democratic Republic of Congo, Eswatini, Ethiopia, Kenya, Kyrgyzstan, Nigeria, Mozambique, Sierra Leone, Tajikistan, Tanzania, and Zambia, ICAP brought its expertise to public health facilities in three new countries in 2021, including Guatemala, Panama, and Kazakhstan.
HIV remains a public health threat in the Central American region. In Guatemala, for example, 9 percent of men who have sex with men and 22 percent of transgender women are living with HIV. Although antiretroviral therapy coverage has been relatively high over the past few years, gaps remain in adherence to treatment and access to PrEP. In partnership with the Centers for Disease Control and Prevention (CDC) and local partners, ICAP supported the introduction of PrEP to publicly supported health clinics in Guatemala and Panama. Through four clinics in Panama, for instance, ICAP helped initiate 300 new users on PrEP after just two months of introduction.
In Kazakhstan, one out of six people living with HIV live in Almaty city. ICAP supported the Almaty Model of HIV Epidemic Control project to introduce a new PrEP program to combat the high prevalence of HIV in the city, enrolling 153 people at risk of acquiring HIV since April 2021.
The power of PrEP to help individuals stay healthy and safe from HIV is undeniable in Kazakhstan and beyond. Alex, a community member that started PrEP, agreed – “I feel safer now that I take PrEP because there are people who either do not know their HIV status or hide it. I worry about not only my health, but also about the health of my potential partners.”
Funder: U.S. President’s Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC) (Central America) and Elton John AIDS Foundation (Kazakhstan)
Project: Programmatic Service Award (Central America); Almaty Model for Epidemic Control (Kazakhstan)
Mentor Mothers Provide a Path to HIV Care in South Sudan
For soon-to-be mothers living with HIV, a mother who has lived through a similar situation can provide valuable guidance, emotional support, and education.
Since 2003, ICAP has supported mothers living with HIV to stay healthy and give their babies the best chance at starting life without HIV infection, including through programs like mentor mothers. From Ethiopia to Burundi, ICAP has brought expertise to 14 countries to support mothers who have used health services to prevent mother-to-child transmission (PMTCT) of HIV to serve as peer mentors to other women accessing PMTCT services.
In South Sudan, a country in which civil unrest has made accessing health care especially challenging, mentor mother support groups are helping to connect women and their families to the care and treatment they need. ICAP supported 115 mothers who have used PMTCT services to serve as peer mentors to other women accessing PMTCT services at 23 health facilities. ICAP trained mentor mothers to facilitate HIV education through group health talks on topics including treatment, breastfeeding, early infant diagnosis, communication skills, and more. The mentors also followed up with mothers who missed clinical visits and encouraged them to bring their newborns to the clinics for early infant diagnosis and care. Since the program began, the number of mothers receiving HIV care and treatment services has more than doubled from 192 in 2018 to 440 in early 2022.
Funder: U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC)
Project: Programmatic Service Award
Research
Generating knowledge, catalyzing solutions
ICAP is at the forefront of research generating new knowledge to improve access to and quality of health services, strengthen delivery mechanisms, and evaluate public health interventions. Leveraging years of experience and a committed cadre of accomplished experts, ICAP designs, implements, monitors, and evaluates a range of innovative implementation science, epidemiological, and clinical research studies. To ensure sustainability of this pragmatic research, ICAP provides training and mentorship in the countries where it works.
Feature Research Story
With a Clinic on Wheels, ICAP Moves Research on Opioids and HIV Into the Passing Lane

In summer 2021, a state-of-the-art mobile clinic began making rounds in the streets of Harlem and the Bronx, drawing attention with its bright graphics. But beneath the colorful exterior is a serious proposition – to address the intertwined public health crises of opioid addiction, HIV, and hepatitis C among people who inject drugs.
Drug overdose is the leading cause of accidental death in the United States, with nearly 108,000 fatalities in 2021, the highest number of overdose deaths recorded in any 12-month period. Factors such as lack of access to health care, poverty, mental health disorders, use of multiple illicit substances, stigma and discrimination combine to increase the risk of HIV transmission and acquisition and other health issues among people who inject drugs.
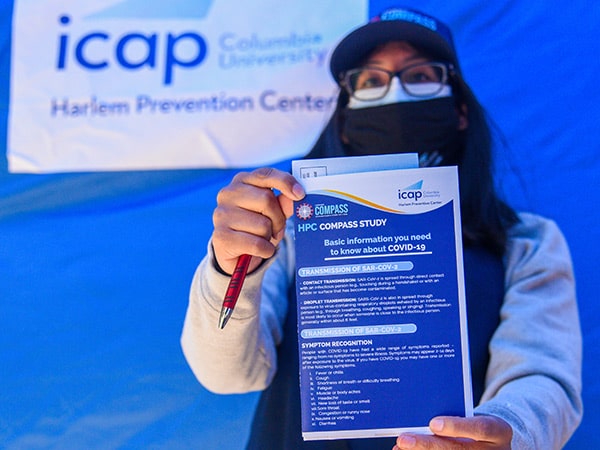
The mobile clinic is at the center of ICAP’s participation in the nationwide INTEGRA study (HPTN 094), which aims to determine whether using mobile health units to deliver integrated health services for people with opioid use disorder can improve addiction, HIV, hepatitis C and substance use outcomes compared to standard of care. At locations frequented by people who inject drugs, ICAP study team members engaged with individuals, provided them with information regarding the study, enrolled participants and followed up with them throughout their study participation.
Participants in the study are randomized to receive integrated care on the “van” – as the study team calls it – or to receive the services of a health care navigator who will assist the participant in finding care in the community.
“The integrated care model means they will be able to receive their buprenorphine [a medication to treat opioid use disorder] prescription from the van,” said Rashaunna Redd, NP, site clinician for ICAP’s Bronx Prevention Center, which conducts the study. “And they will also be tested for HIV, STIs, and hepatitis, and screened for routine primary care problems such as diabetes and blood pressure issues.”
After six months, all participants transition to care in the community. Follow-up after the study extends to 12 months.
“Our goal is to make it as close to one stop as a possible. Although we recognize that some people will have serious medical conditions that require them to see specialists – and we will help them with that,” said Ellen Morrison, MD, site lead at ICAP’s Bronx Prevention Center.
Since the study began, initial findings revealed a high prevalence of mental health disorders such as anxiety, depression, and post-traumatic stress disorder among participants.
“This finding is particularly important because recreational drug use may be used as a form of self-medication,” said Alan Padilla, community educator at ICAP’s Bronx Prevention Center. “Our team is actively promoting the need to address these underlying factors to fully provide addiction services.”
As the van proclaims in bright lettering, ICAP is driving health forward. Mobile health units, along with this study, are providing the engine necessary to reach that mission.
Funder: U.S. National Institute of Allergy and Infectious Diseases (NIAID) with funding from the U.S. National Institute on Drug Abuse (NIDA)
Project: HIV Prevention Trials Network (HPTN); INTEGRA study (HPTN 094)
More Stories
Charting LGBTQ+ Health Challenges in New York City During COVID-19
![]()
As COVID-19 swept the globe, its ruthless trajectory exacerbated the challenges and inequities already faced by the lesbian, gay, bisexual, transgender, and queer (LGBTQ+) community, including employment and housing discrimination, inequitable health care, and more. To gain insight into the burden and impact of COVID-19 on this community, and assess vaccine uptake, ICAP conducted a study that reached more than 1,000 LGBTQ+ New Yorkers aged 18 to 68 years.
While LGBTQ+ individuals in NYC reported a similar burden of COVID-19 and vaccine uptake compared to the general population of the city, the study revealed this community is more likely to experience increased financial and emotional challenges due to the pandemic, particularly among the most stigmatized, such as gender minorities and among those with multiple minority identities. For example, 81 percent of LGBTQ+ individuals reported experiencing financial hardship as a result of the pandemic. This important evidence base will inform strategies to reach unvaccinated individuals and assist policymakers in developing further programs to support those most negatively impacted by the pandemic.
Funder: Rockefeller Foundation
Project: Experiences of LGBTQ+ Populations in New York City During the COVID-19 Pandemic (The LEXICON Study)
COVID-19 and Older Adults in New York City: A Landmark Study

In New York City, older adults had seven times the mortality rate from COVID-19 compared to all other ages, but there was little known about the mental health and social ramifications of the pandemic on this population – especially those who were still living at home and not in nursing homes.
To gain a better understanding of the effects of the pandemic on this vulnerable group, ICAP launched the SARS-CoV-2 Impact on Lives and Views of Elderly Residents (SILVER) study, aimed at understanding the physical, emotional, and economic effects of the COVID-19 pandemic on older adults living at home. A total of 676 participants 70 years and older were enrolled – overall, 18 percent of older adults screened for depression and 17 percent for anxiety, with a greater percent of Latinx older adults reporting loneliness than other races and ethnicities. Almost one-third of older New Yorkers reported financial challenges and almost one in ten reported not having enough to eat.
With new funding, ICAP launched a second SILVER study seeking to learn more about the impact of the pandemic on participants’ ongoing health and wellbeing. The second round of data collection expanded topic areas, pursuing further details about participants’ access to resources such as telehealth, housing, internet, social support, and use of city services. Attitudes towards the COVID-19 vaccine, booster doses, and the influenza vaccine were also evaluated. In addition to following up with the first SILVER study participants, the second study included new participants, specifically Asian New Yorkers, to better represent the diversity of New York City. The ultimate goal of the study was to provide policymakers in New York City and other communities with more accurate information on how to best serve and assist older adults during times of crises.
Funder: New York Community Trust
Project: SARS-CoV-2 Impact on Lives and Views of Elderly Residents (SILVER) Study
Training & Education
Sharpening skills, building capacity
ICAP’s diverse training and mentoring programs enhance the skills of nurses, doctors, laboratorians, lay health workers, and health managers with the goal of addressing critical gaps in human resources for health. By educating and empowering new generations of health workers, ICAP helps to enable strong, sustainable health systems that can effectively serve their populations even in a rapidly changing landscape.
Featured Training & Education Story
From Online to On-site: ICAP Supports Virtual IPC Training in Kenya

At the start of the COVID-19 pandemic, health facilities around the world were faced with infection prevention and control (IPC) challenges, especially in terms of how to safely diagnose and care for patients with COVID-19 and what to do when a health care worker becomes ill. While Kenya has made major gains in recent years in developing guidelines for IPC, such areas as health care-associated illness (HAI) surveillance received limited attention. IPC programs have the potential not only to significantly reduce HAI but also provide important cost savings due to shorter hospital stays and reduced treatment expenses.
To help enhance Kenya’s capacity to prevent, detect, and respond to infectious disease threats in health care settings, ICAP spearheaded an e-learning series for clinicians at two large hospitals in Kenya, Kenyatta University Teaching, Referral & Research Hospital (KUTRRH) and MP Shah Hospital, with the goal of improving critical knowledge on IPC.
Dr. Victor Njom, CEO of KUTRHH, noted the importance of the online campaign not only amid the COVID-19 pandemic, but also as Kenya looks to the future. “We at KUTRRH are proud of our efforts, together with ICAP, to empower frontline health workers with the information that they need in order to more quickly respond to and control emerging threats to public health in Kenya.”
Through peer networks and hospital communication channels, ICAP’s training experts crafted a series of clinician touchpoints at the facilities to motivate them to complete the training modules. Those who completed the modules received certificates of completion and were recognized in small ceremonies for graduates. Thanks to this effort, 62 clinical staff at KUTRRH completed the training in 2021, while efforts at MP Shah Hospital are on track for completion in 2022.
The online trainings, which were co-developed by the U.S. Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO), and the University of Washington Global Health eLearning Program, provide a comprehensive overview of IPC, transmitting knowledge and enabling skills to help reduce the spread of HAI. Modules cover a range of topics, including transmission-based precautions, hand hygiene, waste management and HAI surveillance.
“It is important that all health care workers, both clinical and non-clinical, receive training and supportive resources so that IPC can be implemented at every point of health service delivery,” said Caroline Mwangi, IPC focal person at KUTRRH. “We are grateful for the ongoing IPC trainings and the partnership with ICAP, which ensures that our frontline health care workers are equipped with skills and knowledge to care for patients in the COVID-19 context safely.”
Project: Expanding Efforts and Strategies to Protect and Improve Public Health in Kenya
Funding: Centers for Disease Control and Prevention (CDC)
More Stories
A New Training Program Equips a Workforce to Tackle Health Crises

From hospitals to clinics, COVID-19 overwhelmed health professionals who had not previously had the experience of responding to such an intense and complex health event. As the crisis deepened, it became clear that health professionals require enhanced skillsets to manage health emergencies of this magnitude.
In 2021, ICAP launched the Responding to Epidemics and Crises in Health (REACH) fellowship in collaboration with the Dalio Center for Health Justice at NewYork-Presbyterian. The fellowship is a one-year program for a select group of NewYork-Presbyterian staff to learn how to predict, manage, and lead robust responses to complex health crises, focusing specifically on redeployment from day-to-day duties to health emergency response during a crisis.
The first cohort of REACH fellows graduated in 2022, developing capstone projects that ranged from making redeployment processes more equitable to creating readiness plans for spiritual and emotional support for hospital staff during crises. Over the course of the program, fellows learned from industry experts about topics ranging from U.S. health policy to developing strategies for quality improvement.
“Over the past year, my experience from the REACH fellowship has given me the opportunity to gain a global sense of public health needs and how we can lend better aid to communities,” said Whitney C. Harris, MSN, RN, ACCNS-P, CPNP-PC, manager of Clinical and Community Strategy at Dalio Center for Health Justice and a fellow in the program.
“The COVID-19 pandemic came with many instances of grave news, but the training and education I have received through the REACH fellowship helped me and my colleagues understand how it is possible to triumph through a crisis.”
Project: Responding to Epidemics and Crises in Health (REACH) Fellowship
Funder: The NewYork-Presbyterian Hospital
ICAP Adds Mental Health Training to the HIV Response Toolkit
In partnership with the New York State Psychiatric Institute at Columbia University, psychiatry fellows collaborated with ICAP to develop modules to train health workers on mental health topics to strengthen HIV services. Following a needs assessment survey that queried 250 health workers in nine countries around the world, module topics were tailored to focus on priority areas identified in the assessment. Interactive modules featuring illustrative case studies were developed on topics including communication skills, depression, trauma among children, and more.
“Mental illness and HIV share deep-rooted stigmas, shame, and profound misunderstandings that lead millions to suffer in silence,” said fellow Omar Shareef, MD, MBA. “Through these training modules, this comorbidity is demystified, empowering providers to shine a light on the darkness of living with HIV and mental illness, ultimately delivering their patients a broader understanding of their physical and psychological health.”
Project: ICAP in collaboration with Public Psychiatry Fellowship of New York State Psychiatric Institute at Columbia University
Country-to-Country Visits Energize HIV Program Knowledge Sharing

As countries responding to the ongoing HIV epidemic seek to accelerate progress towards epidemic control, the exchange of practical information about program implementation is a key strategy. Recognizing the impact of in-person visits, ICAP’s Coverage, Quality, and Impact Network (CQUIN) has supported 29 focused country-to-country learning exchanges since 2017.
When the COVID-19 pandemic forced restriction of movement within and between countries, in-person learning exchanges came to a sharp halt. However, as the first wave of the pandemic waned, the CQUIN team established protocols to safely reinstate the visits with admirable results.
During 2021, CQUIN supported five visits between countries – the largest number conducted in a single year.
- Senegal visited Côte d’Ivoire to gain insights into measures the country took to scale up the provision of several months of antiretroviral therapy (ART) medication to patients.
- Burundi also visited Côte d’Ivoire, with a focus on community-based HIV treatment models.
- Côte d’Ivoire visited Eswatini to learn about the country’s approach to differentiated treatment for people with advanced HIV disease.
- Liberia and Kenya visited Nigeria to understand how the Ministry of Health works with private pharmacies to provide community-based ART refills to recipients of care.
Learning visits have a structured approach that is designed to maximize their impact on the visiting country’s HIV program. Topics and travelers are carefully selected, visits are planned in advance with the host country ministry of health, and post-visit action plans and dissemination strategies are supported over time. Visiting teams usually include ministry of health staff, representatives from national networks of people living with HIV, implementing partners, funders, and other stakeholders, who utilize the visits to accelerate learning about new approaches and practical lessons about innovations in differentiated service delivery (DSD) models.
“Resuming country-to-country visits enabled countries to maintain the momentum of DSD scale-up to ensure the resilience of their programs,” said Peter Preko, MBChB, MPH, CQUIN project director.
Project: Coverage, Quality, and Impact Network (CQUIN)
Funder: Bill and Melinda Gates Foundation
Impact Measurement
Strengthening data, enriching analysis
Global health progress depends on reliable data and penetrating analysis to inform policies and target programmatic resources. Across the globe, ICAP undertakes large-scale, innovative impact measurement initiatives, strengthens data quality, and designs and introduces state-of-the-art health information systems that equip ministries of health for evidence-based decision-making around critical health challenges.
*Population-based HIV Impact Assessment (PHIA)
**Tracking with Recency Assays to Control the Epidemic (TRACE)
Featured Impact Measurement Story
Defying the Odds, the PHIA Project Continues to Chart the Global HIV Response

Maria Uwambajimana is one of 1.2 million refugees living in Uganda, which hosts the third-largest refugee population in the world and the largest in Africa. For the first time in the 15 years she has lived in Nakivale refugee settlement, she was tested for HIV.
Uwambajimana participated in the Uganda Refugee Population-based HIV Impact Assessment (RUPHIA 2021), a population-based survey that offers household-based HIV counselling and testing for refugees at selected households. The survey seeks to estimate HIV prevalence and viral load suppression among people living with HIV, as well as collect information on uptake of and access to HIV-related services. RUPHIA 2021 also aims to examine the prevalence of selected behaviors associated with risk for HIV infection, common HIV co-morbidities, and other health conditions.
“Despite Uganda’s pioneering refugee resettlement policies, many refugees and host community members still face challenges accessing basic services, including HIV-related services,” said Dr. Henry Mwebesa, the Ministry of Health’s Director General of Health Services. “This survey will provide us with up-to-date data on HIV burden and other health performance indicators, hence informing our future planning for these communities.”
RUPHIA is one of numerous surveys conducted through the groundbreaking multi-country Population-based HIV Impact Assessment (PHIA) project, which over the last year, has achieved a number of important milestones despite facing tremendous challenges due to the COVID-19 pandemic.
In Mozambique, for example, a fierce cyclone caused major flooding and road blockages that made it difficult for the data collectors to reach remote communities. To ensure the survey was not delayed, the team built wooden bridges to cross over heavy waters.
“Mobilizing quickly to build bridges to help us finalize the survey is an example of creative problem-solving,” said Erika Fazito, a technical specialist on the Mozambique survey, which is known as INSIDA 2020-21. “But it’s also a bigger symbol of this team’s commitment to our mission to capture the state of the HIV epidemic in the most-affected countries, Mozambique included.”
The COVID-19 pandemic affected all planned and ongoing PHIA surveys due to safety concerns and restrictions to gatherings and travel put in place. Nevertheless, PHIA teams, in collaboration with in-country partners and the Centers for Disease Control and Prevention (CDC), were able to forge forward, launching new surveys and completing others. Findings from completed surveys, even in the midst of the pandemic, helped shed light on the status of the HIV epidemic, guiding the way forward for policymakers and program leaders.
In Zimbabwe, the initial ZIMPHIA 2020 results revealed that among adults diagnosed with HIV, 97 percent were on antiretroviral therapy. LePHIA 2020 demonstrated that Lesotho has achieved a 55 percent reduction in HIV incidence among adults aged 15-59 years since the LePHIA 2016-2017 survey. MPHIA 2020 found that Malawi has met the second and third UNAIDS 95-95-95 targets well in advance of the 2025 target date. In Haiti, HAPHIA showed that among those who were aware of their HIV-positive status, 93.3 percent were on antiretroviral treatment, surpassing the second UNAIDS 90-90-90 target for people living with HIV on antiretroviral therapy.
In 2022, ICAP will be launching the second PHIA survey in Tanzania – THIS 2022-2023 – aiming to bring further critical data to inform the ever-more-detailed picture of the global HIV response that ICAP is helping to paint.
Funder: U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC)
Project: Population-based HIV Impact Assessment
More Stories
In Eswatini, Recency Testing Draws a Roadmap for HIV Response Efforts

While 95 percent of people living with HIV are aware of their HIV-positive status in Eswatini, identifying individuals and communities with ongoing transmission is imperative to steer epidemic response efforts to reach those who especially need them. Key programs like Eswatini HIV Recent Infection Surveillance (EHRIS) are providing a roadmap to drive epidemic response efforts by continuously tracking epidemiological surveillance data on person, place, and time of HIV recent infections amongst adults.
Part of the Tracking with Recency Assays to Control the Epidemic (TRACE) program, key insights from EHRIS informed national level policy changes that integrated HIV recency testing with routine HIV testing services. These key policy changes marked important steps to enhance identification of areas with ongoing transmission and accelerate national efforts to achieve epidemic control.
For example, EHRIS revealed young women aged 15-24 years account for nearly half of new HIV infections in Eswatini. As women and girls in sub-Saharan Africa continue to be at a higher risk of HIV infection, this important finding can be used by civil society, community-based organizations, and other stakeholders as an evidence base to inform gender-responsive policies and programs in Eswatini to ensure young women receive the HIV care and services they need to thrive, sooner.
Funder: U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) through the Centers for Disease Control and Prevention (CDC)
Project: Tracking with Recency Assays to Control the Epidemic (TRACE)
COVID-19 Survey in Cameroon Provides Key Information to Navigate Pandemic

To better understand the trajectory of the COVID-19 pandemic, ICAP in Cameroon conducted a time-sensitive surveillance study in collaboration with the Ministry of Health to generate a baseline of SARS-CoV-2 transmission from October-December 2020.
Reaching nearly 10,000 people across the 10 regions of the country, the seroprevalence study was conducted to estimate SARS-CoV-2 antibody prevalence among children and adults aged five years and older. In each region’s capital, three community-based venues, such as markets and transportation hubs, were selected as high-traffic focal points where the research team could survey people of various ages, sexes, and population types. The survey found seroprevalence ranged from 7.5 to 12.4 percent, with higher estimates for those over 50 years old.
“Though the main purpose of the effort was to conduct the survey, there was an emphasis on enhancing laboratory capacity for serological testing,” said Karampreet Sachathep, PhD, who led the survey.
ICAP trained its laboratory partners from the Ministry of Health and partner organizations on how to process and test the specimens as well as to examine the findings.
The findings from the survey provided a baseline measure of the magnitude of the population that had been infected with SARS-CoV-2 at the height of the pandemic when there was limited laboratory-confirmed data. Even in 2022, as the epidemic continues to change across most nations, this evidence-base is critical to guide the future of the COVID-19 response.
Funder: U.S. Centers for Disease Control and Prevention (CDC)
Project: Cameroon National Urban Serosurvey was a community based cross-sectional SARS-CoV-2 serosurvey
Looking Forward
As ICAP approaches it 20-year anniversary, it has set its sights on preparing for the future even while focusing on the challenges of today. This imperative was underscored by the COVID-19 pandemic, a wake-up call for the global community, highlighting the importance of preparedness, capacity, and health equity – so that public health responses reach all people equally.

Pandemic Response Institute Paves the Way to Prepare for Future Health Emergencies

The Road Ahead: Strengthening Global Health Security
Funders
- Amazon
- Baylor College of Medicine
- Becton, Dickinson and Company
- Bill & Melinda Gates Foundation
- Centers for Disease Control and Prevention (CDC)
- CDC Foundation
- Cepheid
- Chevron
- Center for Infection and Immunity (CII)
- Columbia University
- Earth Institute
- Elton John AIDS Foundation
- Emory University
- FHI360
- Foundation for Innovative and New Diagnostics (FIND)
- Fred Hutchinson Cancer Research Center
- GAVI
- Gilead Sciences
- Global Fund to Fight AIDS, Tuberculosis and Malaria
- Global Fund to Fight AIDS, Tuberculosis and Malaria
- Health Resources and Services Administration (HRSA)
- Johns Hopkins University
- Massachusetts General Hospital
- Merck
- Bing Zhao/Harbourview Foundation
- New York Community Trust
- National Institutes of Health (NIH)
- New York City EDC
- New York-Presbyterian
- Orange Foundation
- PPD
- Resolve to Save Lives
- Research Foundation for Mental Hygiene
- Rockefeller Foundation
- United Nations Development Programme (UNDP)
- United States Agency for International Development (USAID)
- Weill Cornell Medical (WCM)
The Road Ahead: Strengthening Global Health Security

Global health threats and emergencies like COVID-19 are no longer a once-in-a-generation threat, as studies estimate people are more likely to experience extreme health emergencies in their lifetime than ever before. With the rise of new infectious diseases, accelerating climate-related emergencies, and antimicrobial resistance, we must look to new strategies and approaches to protect current and future generations.
With a series of initiatives, ICAP is expanding its work in global health security, collaborating with ministries of health, educational institutions, and other partners to bolster the global response to public health threats during the COVID-19 pandemic, and beyond.
In one initiative, ICAP is working in Sierra Leone to ensure that health care workers and facilities are equipped with the training and infrastructure needed to prevent and control infections. In that project, 2,932 health care workers at 450 health facilities were trained on standard infection prevention and control (IPC) precautions – such as waste management practices, appropriate use of face shields and masks, and optimal cleaning practices – leading to a 36 percent increase in health facilities with a dedicated IPC professional.
“The COVID-19 pandemic has put in stark profile the degree to which countries and communities around the world are vulnerable to major health crises,” said Wafaa El-Sadr, MD, MPH, MPA, founder and global director of ICAP. “With these new efforts, ICAP will be drawing on its broad experience and expertise to support advancing global health security that will directly benefit vulnerable regions of the world while contributing to the health and safety of people around the world.”
ICAP’s work on global health security is grounded in the One Health approach, which recognizes that the health of people is closely connected to the health of animals and our shared environment. With increasing climate-related disasters and unprecedented stresses on cities and rural communities, ICAP is partnering with Columbia World Projects (CWP) and Columbia Global Centers (CGC) to convene a global climate-focused network of actors to address and amplify collective concerns, and to guide new pathways to tackle select issues through pedagogical, research, and programmatic approaches.
COVID-19 has proven a wake-up call for global public health, showing the need for increased vigilance, education, and cooperation. Through continued collaboration with partners around the world and a commitment to training versatile health professionals, ICAP is rising to the moment, working towards a future where the security of the world’s health is deeply grounded in the enduring protection and well-being of every individual and community.
“The COVID-19 pandemic has put in stark profile the degree to which countries and communities around the world are vulnerable to major health crises,” said Wafaa El-Sadr, MD, MPH, MPA, founder and global director of ICAP.
“With these new efforts, ICAP will be drawing on its broad experience and expertise to support advancing global health security that will directly benefit vulnerable regions of the world while contributing to the health and safety of people around the world.”
ICAP’s work on global health security is grounded in the One Health approach, which recognizes that the health of people is closely connected to the health of animals and our shared environment. With increasing climate-related disasters and unprecedented stresses on cities and rural communities, ICAP is partnering with Columbia World Projects (CWP) and Columbia Global Centers (CGC) to convene a global climate-focused network of actors to address and amplify collective concerns, and to guide new pathways to tackle select issues through pedagogical, research, and programmatic approaches.
COVID-19 has proven a wake-up call for global public health, showing the need for increased vigilance, education, and cooperation. Through continued collaboration with partners around the world and a commitment to training versatile health professionals, ICAP is rising to the moment, working toward a future where the security of the world’s health is deeply grounded in the enduring protection and well-being of every individual and community.
Pandemic Response Institute Paves the Way to Prepare for Future Health Emergencies

Against a backdrop of increasing health threats and unprecedented strain on health systems in the United States and around the world, the New York City Pandemic Response Institute (PRI) was launched to compile the lessons learned from the COVID-19 pandemic and set the stage for a city that is well-prepared for future major health emergencies, equipped to execute an effective and equitable response. Led by ICAP at Mailman School of Public Health with key partner the CUNY Graduate School of Public Health and Health Policy (CUNY SPH), and a consortium of non-profit, community, and industry collaborators, PRI is set to help reinforce and diversify New York City’s public health infrastructure.
In coordination with the NYC Department of Health and Mental Hygiene and NYC Emergency Management, PRI will work hand-in-hand with New Yorkers in communities across the five boroughs to enhance their capacity to develop locally tailored health solutions, information, and resources to prepare for, respond to, and recover from future health crises.
“One important role PRI will have is creating a deliberate way to listen to communities directly and make sure their input is being brought to the seat of power,” said Mitch Stripling, director of PRI. “PRI will be a place to show clear leadership practices of transparency and accountability, which you need when you’re leading emergency response.”
Anchored in a comprehensive conceptual framework, PRI will address the entire lifecycle of emergency preparedness and response by advancing a dynamic set of activities that increase resilience to the adverse consequences of public health emergencies. Specifically, it will work to:
- Garner involvement from a broad cross-section of New Yorkers and NYC institutions, forming a true whole-of-society effort that empowers local communities;
- Strengthen systems and capacity to respond to known and unknown threats, including through community-led simulation exercises and strategic workforce investments;
- Intervene on the social determinants of health to address racial disparities, promote equity, and improve access to essential care and services in the most affected communities;
- Strengthen prediction of public health emergencies through analysis and monitoring;
- Develop and scale tailored health innovations and technologies;
- Enhance community-led data collection, predictive modeling, and collection and sharing of data; and
- Minimize response times by equipping community organizations and the public with information and resources to take swift action.
PRI’s dedicated team will focus on innovating technologies, tools, strategies, and models to connect diverse city stakeholders to create a city-wide response, and facilitating the development of strategies to inform future preparedness, response, and recovery.
“The Pandemic Response Institute will bring together city agencies, experts across various fields, and nonprofit and for-profit partners to tackle some of the biggest, most intractable public health challenges for New Yorkers,” said New York City Mayor Eric Adams. “I look forward to working with PRI to help grow our public health toolbox with the strategic upstream solutions we need to tackle these crises.”
Mobilizing to Advance Global Health
If 2020 saw the world turned upside down by an unprecedented pandemic, 2021 was the year in which we witnessed massive efforts to address the global health emergency, protect the gains achieved, establish a new normal, and mobilize to confront current and future health threats.
ICAP at Columbia University has been at the forefront of that mobilization – marshalling nearly 20 years of experience and expertise in tackling the most formidable health challenges we face as a global community.
Throughout the past two decades, ICAP has owed its success to a unique model that brings together the design and implementation of effective health programming, world-class research, a commitment to rigorous measurement and evaluation, and innovative approaches to bolstering health systems.
With the COVID-19 pandemic, we saw ICAP’s model tested as perhaps it has never been before. Could we tackle the obstacles presented by having to adjust to the surge of COVID-19? Could we bolster the COVID-19 response around the world? How would we continue to meet the HIV prevention, care, and treatment needs of communities as they faced the urgencies of the COVID-19 pandemic? How would we best be able to protect and support our own staff and colleagues around the world as they performed their lifesaving work?
In this report, we highlight some of the many ways in which ICAP made an impact during a year of enormous uncertainty and extraordinary circumstances. Through innovation, perseverance, and collaboration around the world, we see how ICAP has consistently gone the extra mile to reach those in need, to develop and deploy innovative solutions, to enhance health equity, and to address not just the health emergencies of the moment, but to help put in place systems for the crises to come.
ICAP’s success is anchored in its indelible commitment to partnership. At the heart of everything we do is a commitment to working collaboratively with in-country partners—ministries of health, non-governmental organizations, civil society groups, and community-based organizations. Above all, we never lose sight of the ultimate reason for this work in the first place—the health and well-being of people around the world.
Thank you for your interest and support as we work together towards achieving our mission for healthy people, empowered communities, and thriving societies.
Wafaa El-Sadr, MD, MPH, MPA
Executive Vice President, Columbia Global
Director, ICAP at Columbia University
Director, Columbia World Projects
University Professor of Epidemiology and Medicine
Mathilde Krim-amfAR Chair of Global Health

